Revisiting NuSI, Its Funding by The Laura and John Arnold Foundation, and Its Mission
"NuSI's approach to funding the best scientists in the field without the usual economic and risk constraints is critical for addressing some of the major unresolved questions in human nutrition," said Dr. Ronald Krauss , Senior Scientist for the Children's Hospital of Oakland Research Institute. "The meticulous control and monitoring of diet and energy balance that must be achieved in order to test various hypotheses requires extraordinary resources, and whatever the outcome, this approach is very likely to yield important metabolic information."
By facilitating reliable science to inform dietary guidelines , NuSI seeks by 2025, to see a significant reduction in both the prevalence of obesity and diabetes in the United States. If successful, the resulting impact on healthcare spending in the United States could be reduced by as much as $500 billion annually.
"We are grateful to the Laura and John Arnold Foundation for their continued commitment to NuSI and to lessening the burden of obesity and its related diseases," said Peter Attia, M.D., NuSI President and co-Founder. "Our goals are highly ambitious, and the next three years are just the beginning. {source}

Contributing researchers will span the dietary spectrum, including scientists who personally adhere to veganism; low-carb, high-protein diets; and everything in between. This purposeful “agree to disagree” mix is integral to the success of the project, as biases are discarded in favor of solid, experimental data.
No hidden agenda , no corporate interests, nothing to do with food subsidies or ulterior motives . Just good science. It’s about time, right?
~Tim Ferriss {source}
I could regale you with more, but I think that last quote -- from Tim Ferriss -- pretty much brings down the house. To say there is no agenda here, with all the ties that bind (for starters, here and here), is, at this point laughable.
Acronyms used in this post:
GCBC = Good Calories, Bad CaloriesNHANES = National Health and Nutrition Examination Survey
NuSI = Nutrition Science Initiative (Gary Taubes & Peter Attia)
TWICHOO = Taubes Wrong Insulin-Carbohydrate Hypothesis Of Obesity
USDG = United States Dietary Guidelines
RotL = Review of the Literature
WWGF = Why We Get Fat
The Setup
Stipulation:
Let us accept NHANES data as accurate as presented in the quote from GCBC above. This is, of course, a very controversial stipulation, so if you'd rather use the term hypothetical, do so! But let's say these values are true, because this went into Taubes' "thinking" on the alternative explanation for the obesity epidemic, and NHANES data has been used by most of the anti-USDG forces when framing their arguments. If we average values for the genders then, in absolute amounts, protein and fat intake remained constant and we added about 250 calories from carbohydrate per day (less than 65 grams).
Taubes Posits:
Either calories OR carbohydrates
could account for the increase in weight.
Taubes is basically stipulating here that eating *more* is the cause of the weight gain, his only quandary is whether it is more carb or more calories to blame.
Other Clues from NHANES?
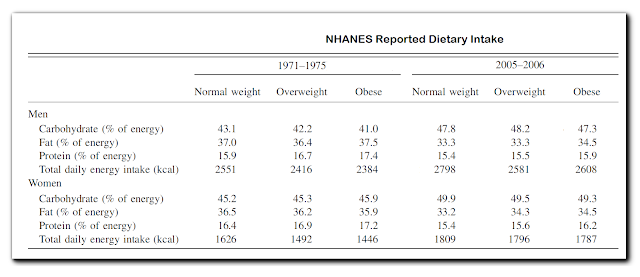
Before moving on, do we have any other data? Yes, or analyses of the same data. The table below as adapted and simplified from a table in this study.
I have seen this held up as proof that calories weren't the issue. After all, the obese consumed less, not more than the lean in NHANES I! I remain hopeful that even the most ardent of low carb advocates, including Taubes himself, does not believe this data is accurate.* But remember our stipulation!
In NHANES I, lean men were consuming 43.1% of 2551 calories as carbohydrate = 1100 calories of carb, while obese men were consuming 41.0% of 2384 = 977 calories of carb. By 2005, lean men were eating 2798 total cals/1337 cal carb while obese men consumed 2608 tot/1234 cal carb. So lean men were eating ~ 250 more total calories and the obese men ~260 more carb calories. It seems very difficult to blame carbs.
In NHANES I, lean men were consuming 43.1% of 2551 calories as carbohydrate = 1100 calories of carb, while obese men were consuming 41.0% of 2384 = 977 calories of carb. By 2005, lean men were eating 2798 total cals/1337 cal carb while obese men consumed 2608 tot/1234 cal carb. So lean men were eating ~ 250 more total calories and the obese men ~260 more carb calories. It seems very difficult to blame carbs.
The Scientific Question:
Still working off the stipulation, how to test this question of excess carbohydrate vs. excess calories? The question is, to use the title of Gary Taubes' 2010 book, Why [Do] We Get Fat? We are looking to isolate cause and effect. The most direct way to do this is to isolate and increase a single potential causal factor, control for all other potential causes, and measure the effect. As carbohydrates represent caloric energy to the human body, it is not possible to manipulate just one of these variables without manipulating another. In other words, I cannot have someone eat more carbs without eating more calories unless I have them reduce intake of another macro. Conversely, I cannot have someone eat more calories but not more carbs, unless I have them increase intake of another macro.
However, since we all agree we're eating *more*, the most direct way to test the higher intake = higher weight hypothesis would be an overfeeding study. Feed a weight stable baseline diet, then add calories as carbs or calories as fat (since this is the basic argument) while keeping protein constant.
This had been done -- in what I would describe as a semi-metabolic ward setting -- seven years before Taubes' groundbreaking New York Times Magazine article, and a full two decades ago! I speak of: Horton et al. 1995. “Fat and carbohydrate overfeeding in humans: different effects on energy storage.” AJCN 62: 19-29.
It is important that everyone reading this understand, that this study included in NuSI's Review of the Literature, a review that is NO LONGER AVAILABLE on the "updated" website.

Transparency ....
"Laura and John Arnold are dedicated to promoting efforts which seek to discover reliable and valid scientific evidence to solve critical problems in our society," said Denis Calabrese, LJAF President. "We believe that NuSI's innovative and transparent model for research will yield necessary answers to drive lasting and positive social impact." source
If you'd like access to this historical document for educational purposes, please request it here. Back to the scientific questions ...
The Horton et.al. Overfeeding Study:
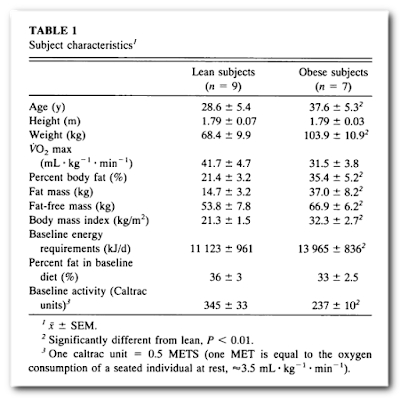
This randomized, crossover study involved 16 lean and obese men, with two 2-week overfeeding periods (150% baseline energy) preceded by 1-week weight stable energy intake, separated by 3 week washout. Subject details in table below.
[I'll include direct quotes from the study to accentuate the "semi-metabolic ward" aspects of this study]
Baseline Energy: Determined from detailed 14 day food diary preceding the experiment.
"We took great care to accurately assess usual energy intake during baseline to ensure that the degree of overfeeding was similar for each subject. After recruitment, each subject completed a 14-d weighed diet diary to estimate their usual food intake. Subjects met with a dietitian and were provided with a set of weighing scales and given detailed instructions of how to accurately complete the diet record by describing types of food consumed and to record appropriate weights. Periodic checks were made to ensure that subjects were completing the record in the required manner."One Week Weight Stable: All foods provided and prepared in metabolic kitchen, tried to mimic subjects personal food preferences, one meal per day consumed at the research center. Intake adjusted if weight was lost.
"One week after completing the diet records, subjects began the first dietary control phase. For 1 wk, subjects were fed a baseline diet reflecting their self-reported habitual intake of energy, fat, carbohydrate, and protein, as assessed from their diet records. The diets consisted, as much as possible, of the foods usually consumed by the subjects and were delivered in a pattern approximating the subject’s usual pattern. Additional food modules (838 kJ), of the same nutrient composition as the diet, were available on request. Use of these modules was previously described (3). This approximated ad libitum feeding. All food was provided and prepared by the Clinical Research Center (CRC) metabolic kitchen, and subjects were required to consume at least one meal at the CRC each day. All other food was packaged to be taken away and eaten in the subject’s home or workplace. Body weight was measured daily during the baseline diet to confirm weight stability. In response to trends to decrease body weight (there were no trends to increase body weight), the dietitian met with the subject to alter the diet plan as needed to reachieve weight stability. "
The baseline diets were not itemized by macronutrients, but based on the fat percentage reported as ~35%, reported mean caloric intake, and assuming ~15% protein, the approximate mean carbohydrate contents of the diets were: 330 g/day for lean and 415 g/day for obese.
Two Week Overfeed: 50% additional calories as all carb or all fat, all foods prepared and provided by metabolic kitchen. 24 hour hospitalization in metabolic chamber on days 1, 7 and 14 of this phase.
Second Overfeed: Following 3 weeks ad libitum normal consumption at home, they were again given 1 week baseline (habitual) diet. This was followed by the 2-week 50% overfeed as described above of the other macronutrient. Order of overfeeds was assigned at random.
The approximate carbohydrate intake during the overfeed would be 660 g/day for lean and 830 g/day for obese.
Second Overfeed: Following 3 weeks ad libitum normal consumption at home, they were again given 1 week baseline (habitual) diet. This was followed by the 2-week 50% overfeed as described above of the other macronutrient. Order of overfeeds was assigned at random.
The approximate carbohydrate intake during the overfeed would be 660 g/day for lean and 830 g/day for obese.
Main Outcomes: So as not to clutter this post with a detailed discussion of macronutrient balance, energy expenditure, etc., I am simply going to provide the table of body composition changes and repeat the conclusions from the abstract:
From energy and nutrient balances (intake-expenditure) we estimated the amount and composition of energy stored. Carbohydrate overfeeding produced progressive increases in carbohydrate oxidation and total energy expenditure resulting in 75-85% of excess energy being stored. Alternatively, fat overfeeding had minimal effects on fat oxidation and total energy expenditure, leading to storage of 90-95% of excess energy. Excess dietary fat leads to greater fat accumulation than does excess dietary carbohydrate, and the difference was greatest early in the overfeeding period.
NuSI's Review of the Literature and Horton et.al.
Taken on its own, Horton et.al. would by no means be a definitive study on what causes obesity. It suffers from:
- Being a single study.
- Short term overfeed: Could be insufficient to detect small differences that would be meaningful accumulated over a longer term. Could also be within a transitional time frame for adaptation, and differences observed could diminish, disappear, increase or even reverse over time.
- Overfeed (50%) is significantly greater (more acute) than the NHANES increase in the 10-15% range. Thermogenesis may not be linear dose/response.
- Small sample. This is somewhat compensated for by cross-over design (e.g. better than comparing two separate groups of 16 subjects). Even smaller samples for comparing just lean or just obese subjects.
- Not a metabolic ward study. Although one might expect less cheating than in an extreme underfeeding study, there's still the possibility of subjects not consuming all foods, or of consuming non-study foods.
The methodology of Horton is pretty solid to directly test of the hypothesis of Gary Taubes. That is, what caused the obesity epidemic: Was it the carbohydrates or the calories? Put another way, was it the quality of calories or the quantity of them?
When NuSI set out to change the world in Manhattan Project (cough cough) style, they outlined what was "wrong" with the existing science. Much of this was stating the obvious limitations for study size, duration and supervision. Presumably, NuSI's millions were going to fix these "problems" and thus do "good science". In this light, it is instructive to peruse NuSI's review of the literature circa 2012 and see how they described various studies or the grounds upon which they were dismissed as "bad". Remember, all of this research has gotten us *no* closer to any answers according to Gary Taubes and Peter Attia.
I encourage you to look at the full file, I can't screen shot significant portions and have it be readable. Here is the description of Horton et.al. It raises a few questions.
In the Experimental Conditions (middle right), this is described as "free-living, plus occasional 24-hour calorimeter". While this is technically true, descriptions in other studies were inconsistent using terms such as "feeding study". It should have been noted that all foods were prepared and provided and some mention of the care taken to match usual diets and energy intake on an individual basis. This is far different from many other studies. In my opinion, this is more than mere oversight, but an attempt to diminish the higher quality aspects of some of the existing studies.
So far, we could "fix" what's wrong with this study by:
- Confining subjects to a metabolic ward and monitoring intake
- Extending the length of the study
- Increasing the number of subjects -- this would likely need to be increased significantly as a longer study time would almost necessitate a group comparison vs. crossover design.
But there was nothing wrong with the study design per se. So now, here comes a clever dismissal ...
No significant differences between diets or groups in body weight or body composition changes. Between the two diets, fat overfeeding gained 1.51 kg in fat mass, compared to 1.48 kg. Total energy expenditure was consistently higher on the carb overfeeding, as measured by calorimeter, and fewer of the excess carb calories were stored by this estimate.
First of all, on what basis does this outcome provide no meaningful information? On what basis can this "black swan" for TWICHOO be written off? More on that in a bit. But one of the most hyped things about NuSI's supposedly groundbreaking science will be the use of metabolic chambers.
Caption: The Arnolds are focusing their generosity on big-picture problems like obesity, including funding a major study on the topic headed up by Dr. Peter Attia, pictured here in a metabolic chamber.
Go look at the discussion in Horton. This is what they did for three 24-hour periods during each 14 day overfeed (Days 1, 7 and 14). The way NuSI worded this outcome, it was an "estimate" that yielded the result, with the distinct whiff of dismissal. Billionaire backing doesn't make science better ....
NuSI's Comments/Takeaways for Horton: (numbering mine)
- Hypercaloric diet, 14-day trial, adding 50 % excess carbohydrates or fat to a baseline diet that could already be carbohydrate-rich.
- Neither diet would reduce insulin levels below baseline.
Let's address these separately.
1. Baseline Diet was Carbohydrate Rich:

Now this review of the literature was billed as a comprehensive overview of the science. Someone or someones, with at least the blessing of Taubes and Attia, went over the literature with a fine tooth comb. How is it possible that they can't definitively say that the baseline diet in Horton WAS already carbohydrate-rich? I've shown that enough information is available for a reasonable estimate to be made, and the person summarizing this study should have been able to do this. This makes one wonder how closely all of this literature was scrutinized? Did they perhaps miss a few definitive answers along with some study details? Or at least some points for further study??
The baseline carbohydrate level is irrelevant to whether an increase in carbs causes weight gain irrespective of calories. In this study significantly more carb was added on top of carb intake similar to that in the 1970's (slightly more), and it did not cause more weight gain compared with the same amount of calories as fat. In the 1970's men were consuming between 250 and 300 g/day of carbohydrate, which is well above any "threshold" for a diet to be considered low in carbohydrate. The increase by 2005 was 200 calories (net 150 = + 200 carb - 50 fat) or 50 grams of carbohydrate. The assertion is that increasing 250-300 g carb to 300-350 g carb caused the weight gain. In Horton, the increase in carb intake was drastically more, essentially doubling intake from baseline. At least in this study, this produced no greater effect than an equal caloric amount of fat.
The "high" carbohydrate intake at baseline was often used as a way to dismiss this study back in the glory days of alpha glycerol phosphate rule. Recall, a key component of TWICHOO put forth in GCBC was that you can't store fat without dietary carbohydrate. Back then, anyone citing Horton would be told that had all calories been protein and fat in the overfeed, the subjects would not have gained weight. Even if this were true, it would be irrelevant. Americans ate considerable carbohydrate in the 1970s. Americans added carbohydrate to this considerable baseline intake.
2. Interventions Would Not Reduce Insulin Levels
The second "disqualifier" that the diets were not designed to reduce insulin levels is specious. This was not the purpose of the study, for starters. Secondly, we are not talking dietary interventions to provoke weight loss. However, again the NuSI reviewer(s) fell asleep at the switch when they wrote this, because oddly enough (it is unexpected), the fat overfeed in the lean men did produce a considerable drop in fasting insulin levels. But equally damning for TWICHOO, these same lean men saw a considerable increase in fasting insulin during the carb overfeed. Combined, these opposite changes in insulin make for quite a "swing" in insulin levels between the two interventions and should have dramatically favored carb overfeed to the fat overfeed for weight gain. This did not happen. Why did the NuSI reviewers ignore this?
The NuSI Mission and their Review of the Literature:
From the same article cited earlier,
I would like to believe that the NuSI RotL was indeed intended to be a gut check on where nutrition science stood on key issues of the day with the eye on building upon, not discarding out of hand, the existing body of work. "No definitive answers" is still not "no answers whatsoever". Any good scientific endeavor involves assessing where you're at. It usually does not necessitate reinventing the wheel entirely, but rather looking at ways to improve, refine, and ... sometimes just repeat some past work.
When NuSI unveiled it's research, there were three studies to be funded by the initial grant:
- Energy Balance Consortium - uncontrolled, pilot met ward study on energy expenditure in keto vs. normal diet
- Stanford Study - 1 year VLF vs VLC free living in 600 people
- Boston Children's Hospital Study - now redubbed Framingham State Food Study
#1 was completed sometime last year and we await results of the *pilot* study. It will tell us nothing actionable for dietary guidelines for the general public or the obese. A ketogenic diet has therapeutic usefulness or potential usefulness in a rather more narrow scope that stated by staunch advocates. It's hardly the first time any of the participating researchers have employed various methodologies or equipment. #2 according to clinicaltrials.gov really is mostly employing an app to track intake, but is hardly first of its kind in any meaningful way. Which leaves us with #3, which should be retitled Ebbeling II. It is hardly novel, and the experimental design of Ebbeling I leaves a lot to be desired as pertains to relevance to real world problems and strategies.
First-of-Its-Kind? What exactly about the Ludwig/Ebbeling/NuSI study is "first of its kind"? I've C&Pd the clinicaltrials.gov descriptions to save you the digital trips.
Original Study
For most of the last half century, reduction in fat intake has been the primary nutritional approach for the prevention and treatment of obesity and cardiovascular disease (CVD). Over the last few years, very low carbohydrate (Atkins-type) diets have achieved great popularity, with publication of several studies suggesting greater weight loss and improvements in CVD risk factors over 3 to 6 months. Recently, a third dietary approach focused on glycemic index (GI) has generated interest. However, few studies have compared the effects of these diets on body weight regulation and risk for CVD. The primary hypotheses of this study are that any diet that lowers the postprandial rise in blood glucose (very-low-carbohydrate or low-GI) will have beneficial effects on the physiological adaptations to weight loss and on some CVD risk factors. However, other CVD risk factors will be adversely affected by a very-low-carbohydrate vs. a low-GI diet. Preliminary data provide strong support for these hypotheses, by showing that resting energy expenditure declines less and CVD risk factors improve more with weight loss on a low-glycemic load diet compared to a conventional low-fat diet. This application proposes a cross-over feeding design to study the effects of three diets following 12.5% weight loss in obese young adult subjects (n = 24, age 18 to 40 years). The diets are: 1) conventional low-fat, with 60% carb, 20% fat, 20% protein; 2) low-GI with 40% carb, 40% fat, 20% protein; and 3) very-low-carbohydrate with 10% carb, 60% fat, 30% protein. The primary outcome is resting energy expenditure (indirect calorimetry). Secondary outcomes include total energy expenditure (doubly labeled water), thermic effect of food (indirect calorimetry), physical activity (accelerometry), insulin resistance and B-cell function (frequently-sampled OGTT), blood lipids, blood pressure and measures of systemic inflammation and coagulopathy. This study should have major public health implications to the millions of Americans currently following diets to decrease body weight and risk for heart disease.
NuSI Study
Many overweight and obese people can lose weight for a few months, but most have difficulty maintaining weight loss over the long term. One explanation for the poor long-term outcome of weight-loss diets relates to behavior, in that motivation to adhere to restrictive regimens typically diminishes with time. An alternative explanation is that weight loss elicits biological adaptations - specifically a decline in energy expenditure and an increase in hunger - that promote weight regain. The purpose of this study is to evaluate the effects of dietary composition on energy expenditure and risk for chronic diseases, while also exploring physiological mechanisms underlying these effects. The study will be performed in collaboration with Framingham State University, providing a novel and feasible method for feeding subjects in dining halls and monitoring compliance.
Following 12±2% weight loss on a standard run-in diet, 150 adults (aged 18 to 55 years) will be randomly assigned to one of three weight-loss maintenance diets controlled for protein content (20% of energy) and varying widely in dietary carbohydrate-to-fat ratio: Low-carbohydrate (15% of energy from carbohydrate, 65% fat), Moderate- carbohydrate (40% carbohydrate, 40% fat), High-carbohydrate (60% carbohydrate, 20% fat). During the weight-loss maintenance phase, energy intake will be adjusted to prevent changes in body weight. The primary outcome will be change in total energy expenditure (indirect calorimetry using stable isotopes) at 20 weeks. Secondary outcomes during weight maintenance will include energy intake, resting energy expenditure (indirect calorimetry using respiratory gas exchange), physical activity (accelerometry), measures of insulin resistance and skeletal muscle work efficiency, components of the metabolic syndrome, and hormonal and metabolic measures that might inform an understanding of physiological mechanisms. We also will assess voluntary food intake and weight change during a 2-week ad libitum feeding phase, as an objective measure of dietary effects on hunger. The analytic framework for addressing study hypothesis will be repeated-measures analysis of variance, with adjustment for covariates (sex, race, ethnicity, age, anthropometrics). We also will test each covariate for effect modification (covariate × diet interaction).
So what was the purpose of the NuSI RotL? It's somewhat beyond belief that anyone would look at all that has been done for the sole purpose of saying "this is all crap", and yet this seems to be exactly what they've done. Why didn't they instead look at all of these studies and find the good parts to build upon to design that study? Here's where their bias prevents a truly scientific inquiry. Because rather than building on any of this, they discard it all and throw their largest grant at Ludwig's research group.
Now I'm not going to bat for any particular scientist or research group, but I am suggesting that NuSI has not shown much promise here in the early going at identifying any truly different approach. It boggles the mind that the Energy Consortium study was a "pilot trial" at all. All that money wasted really. We might get some useful information on mechanisms and such, perhaps put some myths to rest (though if the response to Kevin Hall's recent study is any indication, don't hold your breath). But in the end, a larger scale longer study would be needed begging the question of why not just start there?
But what we need is NOT another weight loss study at all, or ever. What we need is a weight gain study.
So repeat Horton et.al. Only ....
- More subjects
- Longer duration
- Smaller excess (perhaps 25%)
- Measure REE/TDEE at regular intervals, use most accurate and perhaps redundant means of doing so.
- Greater accountability of intake
- Match digestive bioavailability of calories (by which I mean ideally formulas would take this out of the equation, but for a long term study and real world applicability, real foods are a necessity -- let's not do 3000 calories of almonds then OK?)
It might be beneficial to add two more study groups -- you know, for a definitive answer to it all. These would be isocaloric to baseline TDEE only replace 25% carb with fat in one group, and in the other replace 25% fat with carbohydrate. THIS would be a comprehensive head-to-head on what makes us fat.
NuSI would have zero interest in this. Neither, apparently would the Laura and John Arnold Foundation and any of its various related subsidiary "philanthropies". David Ludwig has already written the book (affiliate link).....
Transparency ....







Comments
Post a Comment
Comment Moderation is ON ... I will NOT be routinely reviewing or publishing comments at this time..