Scientist Bashing II ~ The only sport approved by your favorite VLC guru?
As mentioned in my first rant on this issue, I had intended this post to be part of it. But it's a somewhat different topic -- condescension of gurus sporting MD's against those lowly PhD's, or "just scientists" in general -- and lengthy enough (per my usual - grin) in its own right.
A short while back, Dr. Mercola weighed in on the whole "safe starch" debate. However collegial the meeting at the WAPF conference between Paul Jaminet and Mercola, it did not keep Mercola from taking pot shots. The evolution of the title of the piece is interesting in and of itself. Mousing over the tab on my browser, and the URL reveal the original title: "Experts Discuss The Benefits of a Low-Carb, High-Fat Diet", but on the actual post? Initially it was: "Expert_ {singular} Explains Why You Don't Need Non Fiber Carbs". Huh? That sounded strange for a post that prominently displayed the PHD Apple/Plate, but OK. But shortly after that it was changed to: "These Two Natural Foods Will Throw Your Blood Sugar Out-of-Whack". Well, that's more what you might (or what I might expect) from Dr. Mercola. Although Mercola seems to be receptive to Paul & Shou Ching's diet, it is clear which side he comes down on and who he feels is the real "expert" here: Rosedale. If there was any doubt, here is what Mercola says almost from the get go:
A short while back, Dr. Mercola weighed in on the whole "safe starch" debate. However collegial the meeting at the WAPF conference between Paul Jaminet and Mercola, it did not keep Mercola from taking pot shots. The evolution of the title of the piece is interesting in and of itself. Mousing over the tab on my browser, and the URL reveal the original title: "Experts Discuss The Benefits of a Low-Carb, High-Fat Diet", but on the actual post? Initially it was: "Expert_ {singular} Explains Why You Don't Need Non Fiber Carbs". Huh? That sounded strange for a post that prominently displayed the PHD Apple/Plate, but OK. But shortly after that it was changed to: "These Two Natural Foods Will Throw Your Blood Sugar Out-of-Whack". Well, that's more what you might (or what I might expect) from Dr. Mercola. Although Mercola seems to be receptive to Paul & Shou Ching's diet, it is clear which side he comes down on and who he feels is the real "expert" here: Rosedale. If there was any doubt, here is what Mercola says almost from the get go:
I had a chance to listen to Dr. Jaminet at the Dallas Weston A. Price Conference and was impressed with his ability to consolidate research information.
However he is only a Ph.D. researcher, an astrophysicist, and his wife Shou-Ching is a Harvard biomedical scientist who does not personally treat patients.
Paul is "only" a PhD researcher, and Shou-Ching? Well he links to her profile, but why not mention that she is also a PhD researcher? Even of she is "only" one. This is a dis. Here is what Shou-Ching does:
Experimental research:1. The functional role of TM4SF1 in tumor angiogenesis;2. The study of molecular mechanisms in a surrogate tumor model of adenovirus-VEGFA-induced angiogenesis in mouse ears, in order to identify new biomarkers for angiogenesis that can potentially be used as targets for cancer therapies.
Clinical research:1. Development of routine tests for early detection, prognosis, prediction of response to treatment, monitoring of cancer progression, and molecular validation of drug treatments of CLL (Chronic Lymphocytic Leukemia).
But neither treats real patients so it's the MD who is the better "expert" in Mercola's eyes. But clearly it has to be more than just an MD that makes one an expert. After all, Mercola and Rosedale are among a select few doctors who routinely lambaste the other 99.9% of practicing MDs. You know ... all those other MDs blindly accept "conventional wisdom" and don't really get the science or believe in fatally flawed science. According to Rosedale's site, he's all about "bridging the gap between science and medicine". As far as I'm concerned, Rosedale, Mercola or any other MD out there is no more or less qualified to distill biomedical research than any other person graduating from college with a science degree, and nowadays more and more doctors don't even come from a scientific undergraduate background. "On average", anyone going further on the research track, even in an unrelated science, is likely more qualified to critically review peer-review research than an MD. The skill sets applied on a daily basis are just different. (Disclaimer: Again not intending to offend, there are many lay people who have demonstrated abilities in this regard, just saying "on average")
I've made no bones about Rosedale pegging my BS-meter. I'm sorry if it annoys my critics, but I have no patience for those who just make stuff up and seek to educate all of us dopes with their revolutionary wisdom. Rosedale claims to know the science, and has repeatedly said that I do not. What does he base his superiority on? His clinical experience. You see, because I've never ordered a leptin test on a patient, I'm incapable of understanding the leptin research ... or something like that. Which is pretty rich from someone who claims that leptin "spikes" when you eat carbs, despite clear and consistent evidence to the contrary. I have repeatedly challenged Rosedale to provide references that support his contentions. To his credit, unlike his alter-leptin-ego, he at least tries to provide some evidence rather than sending me dismissively off to "do my own research" and go read a biochemistry book. But the research he cites is woefully inadequate and his interpretation is misleading and often flawed ( ... and I've shown you why!).
I had taken on two of the references he put forth to argue that we're all going to die from our blood glucose. One of those was an analysis of stroke risk from the Whitehall prospective study that measured 2 hr. glucose levels after a 50g glucose oral glucose tolerance test. This was the subject of: Keep the Leptinade flowing! I'm going to die from my glucose anyway .... I would encourage folks to go read that post, though I will hit the highlights in my discussion here in a bit.
In his re-re-re-whatever-buttal, Rosedale made the following comment in response to this (I put Paul in grey, Rosedale in black:
This study looked at blood glucose levels 2 hours after swallowing 50 grams of glucose, and then followed the men for 38 years to observe mortality rates. CarbSane makes an important observation: this study used whole blood rather than plasma to assay blood glucose. Whole blood has more volume (due to inclusion of cells) but the same glucose, and so less glucose per deciliter. According to this paper, standard (plasma) values are about 25 mg/dl higher, so 95 mg/dl in whole blood actually corresponds to a plasma value of about 120 mg/dl.
That was a 1965 paper. There have been considerable advances in the measurement of glucose since then, such that the differences are less, though still present. Actually, to convert from whole-blood glucose, multiplication by 1.10 (~10% difference) has been shown to generally give the serum/plasma level…
From the Joslin Diabetes Center at Harvard website; “The difference is that plasma numbers read about 10 – 12% higher than the older whole blood numbers. So if your fasting and pre-meal blood glucose target is 90 – 130 mg/dl plasma glucose, it would be 80 – 120 mg/dl if your meter reads whole blood.”Here's his dig at yours truly:
Though this is known among clinicians in the field, without having clinical experience, CarbSane would not know this.
Well, it is true dear readers. I have exactly zero experience as a clinician. You would think this should hold up for Rosedale to allow a response from this piddly blogger on his website, but not so. So smugly sure of himself is Rosedale, that he censored the following comment I tried to submit:
Apparently Rosedale has never had to do any sort of comprehensive review of historical literature, often containing conflicting reports, and try to reconcile the meaning of data. I have. From all I've read on the topic of appropriate postprandial BG's to and OGTT, the cut-offs in this study just seemed awfully low on first read. Rather than try to pass off that needlessly alarming data, I immediately looked for the context. As stated in my comment, Rosedale's contention that the correct adjustment based on current measurement techniques is just wrong. Let's assign some letters for clarity: A = 1965 blood glucose, B = 1965 plasma glucose, C = 2011 blood glucose, D = 2011 plasma glucose. Rosedale is trying to convince you that the C-to-D conversion factor is more appropriate than the A-to-B conversion factor because analytical science has progressed to better tests. But this is exactly why I was happy to find the 1964 reference so quickly, because it is that conversion that is relevant vis a vis blood levels measured in 1965.
If Rosedale's point is that current methods are more accurate than older ones, then we need a conversion factor of A-to-C or B-to-D. To do that, one would have to take identical blood and plasma samples, analyze them by 1965 methods and 2011 methods and compare the results. If the quality of the tests has introduced error here, using a modern conversion factor of blood v. plasma levels would only compound that error if anything. And ultimately, Rosedale wants you to use current C-to-D conversions to equate A-to-D. Nah na nah! No serious scientist would suggest such a thing. Rosedale does make a good point (though I don't think this is what he's concerned about), that it is important to remember these results were obtained by likely less accurate means available in 1965. Any extrapolations to today's data should be done with caution -- those would include extrapolations he might make as well!!
Before I move on, one more point on those 2hr BG levels. They were for 50g OGTT not the 75g OGTT that is used most often today. While the blood glucose spikes are "dose dependent", and insulin response to glucose is also "dose dependent", this does not mean there is a perfect relationship or 1:1. One would expect a 50% higher glucose and insulin response to a 50% higher glucose load, but we don't see this because insulin is secreted to prevent this very thing. In one study I found, 1 hr levels were essentially the same following both OGTTs (I'll discuss some of the interesting data I've come across comparing the two OGTTs in a future post), but it is not unreasonable to expect somewhat higher responses in both following 75g glucose vs. only 50 grams. Suffice it to say that Rosedale doesn't even account for the fact that a different dosage was used for the OGTT. Perhaps you need to be a research scientist with experience in both generating and analyzing clinical data, rather than just ordering up the tests to know this is important ...
If Rosedale's point is that current methods are more accurate than older ones, then we need a conversion factor of A-to-C or B-to-D. To do that, one would have to take identical blood and plasma samples, analyze them by 1965 methods and 2011 methods and compare the results. If the quality of the tests has introduced error here, using a modern conversion factor of blood v. plasma levels would only compound that error if anything. And ultimately, Rosedale wants you to use current C-to-D conversions to equate A-to-D. Nah na nah! No serious scientist would suggest such a thing. Rosedale does make a good point (though I don't think this is what he's concerned about), that it is important to remember these results were obtained by likely less accurate means available in 1965. Any extrapolations to today's data should be done with caution -- those would include extrapolations he might make as well!!
Before I move on, one more point on those 2hr BG levels. They were for 50g OGTT not the 75g OGTT that is used most often today. While the blood glucose spikes are "dose dependent", and insulin response to glucose is also "dose dependent", this does not mean there is a perfect relationship or 1:1. One would expect a 50% higher glucose and insulin response to a 50% higher glucose load, but we don't see this because insulin is secreted to prevent this very thing. In one study I found, 1 hr levels were essentially the same following both OGTTs (I'll discuss some of the interesting data I've come across comparing the two OGTTs in a future post), but it is not unreasonable to expect somewhat higher responses in both following 75g glucose vs. only 50 grams. Suffice it to say that Rosedale doesn't even account for the fact that a different dosage was used for the OGTT. Perhaps you need to be a research scientist with experience in both generating and analyzing clinical data, rather than just ordering up the tests to know this is important ...
The diagnosis of diabetes, by conventional standards, (though I believe that diabetes ought to be diagnosed by insulin and leptin values rather than blood glucose), is defined as a fasting plasma/serum measurement of 126. Using the conversion factor that Jaminet indicates would translate to a blood monitor level of 101. That, in turn, would translate to a whole lot more diabetics, that may benefit to a greater extent, as he mentioned in Jimmy Moore’s post, by using a more “diabetic” diet such as mine. My statement that we all should be treated as diabetics would start to ring true.
There is no significant difference in mortality among any group with post-challenge whole blood glucose up to 5.29 mmol/l (95 mg/dl), corresponding to 120 mg/dl or 6.7 mmol/l in standard measurements..
(…or 105 mg/dl if the correct conversion factor was used.)
Well, the correct factor was used. Rosedale is in clear error here. And further correction for the dose is required to truly put this into proper context. In response to the challenge, Rosedale just chants: Dia betes ... Dia betes ... Betes betes ... Dia dia ... Dia leptin ... Dia leptin ... Leptin Leptin ... Dia dia*
My [Jaminet] interpretation: This study wasn’t designed to observe the lower end of the U. At the higher end, it is consistent with the other studies: mortality rises with 2-hr plasma glucose above 120 mg/dl.
Actually in this study, mortality correctly rises significantly above 95 mg/dl blood, but that correlates to 105 mg/dl plasma if the much more modern and accurate conversion of 10% is used. This again is far lower than the 140 mg/dl that Jaminet has deemed safe. {Rosedale bolded this, I've bolded/italicized differently for emphasis}
Repeating his incorrect assertion of what is the more applicable conversion factor doesn't make him right. The appropriate conversion factor is that which was carefully examined and documented at the time. But the "correctly" does reveal the bias ...
Rosedale seems to base his entire argument from this study on the statement from the abstract below:
Plots of stroke mortality rates versus blood glucose identified an upward inflection in risk of death from stroke at about 4.6 mmol/l. This upward inflection in risk could be adequately described using a single linear term above this threshold.
We are not provided with those plots. Bad, bad science!!! Oh shut up CarbSane. There I go talking to myself again. What we do know is that they divided the bottom 90% of the subject's data into 3 equally sized groups of 30% each and that there was NO difference in stroke or all cause mortality between the bottom third and the top third of these groups, across the groups, backwards, forwards or upside-down. NONE. For overall mortality rate they were 30.4, 30.6, 30.5 and for stroke they were 2.7, 2.9, 2.7 -- for bottom to top thirds respectively. Sixties, nineties and beyond, this sort of comparison within strata of a population hold meaning, though still need be viewed with caution when population shifts occur.
Returning to the study, apparently, despite the fact that
"preliminary analyses showed that the main increase in stroke mortality rates was above the 90th percentile of blood glucose distribution"
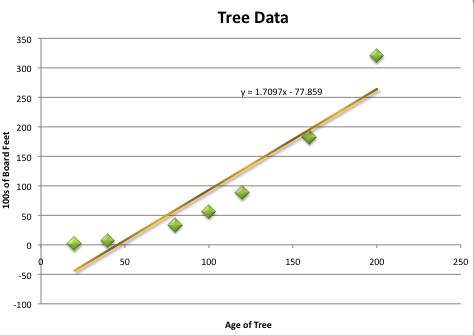
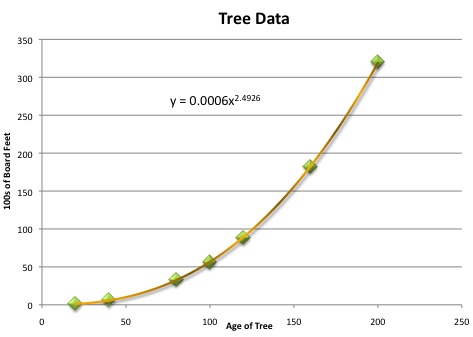
... the study authors decided to nudge the lower limit of the data included in a plot to where a linear model would still hold. This, seems to be where the 4.6 mmol/l "threshold" comes from. All I can say to that is that the bolded/italicized "adequately" qualifier above says it all. Below are some plots of tree growth data from this discussion of modeling. The two plots just so happen to illustrate my point perfectly:
Clearly the plot above right more closely describes the relationship between the two variables, but the line on the left may well pass statistical muster to "adequately" describe the same relationship. This scientist is more compelled by the data that this study DID present, than that which they didn't, and doesn't sound all that convincing. {The visuals on the data table they did share are misleading. They broke it out into 7 columns with relative risks compared to the lowest column so it was visually more narrow. The result? Ninety percent of the people are in columns that are less than half of the table while 10 percent make up more than half. This is not deceptive per se -- they explained it in the text -- but the more casual observer can't help but get sucked into the exaggerated mortality changes in the right 4 columns. I wonder why they didn't break the top third of the 90% into two groups. Show me the money!}
The last part of Rosedale's piece addressing the study was:
My [Jaminet] interpretation: This study wasn’t designed to observe the lower end of the U. At the higher end, it is consistent with the other studies: mortality rises with 2-hr plasma glucose above 120 mg/dl.
Dia betes ... Dia betes ... oh stop that chanting!!Actually in this study, mortality correctly rises significantly above 95 mg/dl blood, but that correlates to 105 mg/dl plasma if the much more modern and accurate conversion of 10% is used. This again is far lower than the 140 mg/dl that Jaminet has deemed safe.
Here's where any analysis by Rosedale wouldn't pass a peer-review smell test. You simply CANNOT take ANY results of a 2 hr. single OGTT and extrapolate it to any inferences as to what constitutes a safe glucose level at any given time. I think this is the trap Paul Jaminet has fallen into as well -- identifying 140 mg/dl as a cut-off. That value comes from a study on analyzing fasting blood glucose, FBG. The very fact that there are folks who have elevated fasting glucose but normal postprandial glucose tolerance, and vice-versa cautions us strongly against drawing inferences for one parameter based on the other. (mucho in the pike on this topic as well). You see, what all of those idjut diabetes researchers know, is that endogenous glucose production (gluconeogenesis in the liver) is the biggest contributor to chronic hyperglycemia and the resulting complications thereof.
Bottom line, let's say I measure my blood glucose and it's 160 mg/dl. Should I worry? It really does depend. This idiocy from the likes of L. Ron and WheatBelly that you're going to glycate yourself to blindness is just that: idiocy. If that measurement was done within an hour of a huge starchy meal, especially if I had a big fatty meal the night before, it might be considered a rather awesome display of my insulin sensitivity. If, on the other hand, it was a fasting level, then I'm diabetic. Does that make the glucose, itself, directly responsible for the complications we see? NO. And I'm not saying that glucose per se doesn't have toxic effects. But context is everything. The uber-hyperglycemic mouse, LIRKO, appears to deteriorate mostly because its poor liver can't keep up with the unchecked gluconeogenesis. Despite rampant hyperinsulinemia and hyperglycemia for many months, the latter subsiding as the liver begins to fail, the mice don't seem to be banging into the walls of their cages and making extra bucks selling jam made from their urine.
Let's hold these gurus up to the same standards they say are insufficient to keep scientists honest. I would like to see Rosedale take the same data, without the conclusions of others, and analyze it. Then present it and try to convince a "jury of peers" that we are all diabetics to some degree, and there is no "safe" level of blood glucose below which we can escape the ravages of aging. It would get kicked to the curb. But he'll be hawking two books sometime soon. Stay tuned to his FB page!! Too bad they won't be vetted critically on the science he claims to hold so dear.
To Conclude: When an MD refers to someone as "just a PhD", even in an unrelated field, beware! When those same types make you wonder if the "D" in their designation stands for Doctrinaire instead of Doctor, be doubly aware. When they bash other docs or scientists ... challenge them to provide that elusive body of evidence upon which they base their revolutionary proclamations. Rosedale did not disappoint in providing ample evidence that he brings a box cutter to a sword fight in this realm.
Folks like Rosedale talk a good game. Nameless, and even named, representatives of "Conventional Wisdom" are somewhat easy targets for them. Often those targets are constrained in their ability to respond. Don't give the Rosedales of the world a free pass. They should have just a few references at the ready, after 20 years of looking at these things after all, to convince you of their own wisdom. When they do not, it speaks volumes. And repeating the same claims doesn't make them hold any more water.
*All together now ... Let's cue George Harrison's "My Sweet Lord" and sing the Maha Mantra fade out L.Ron style:
Dia betes ... Dia betes ... Betes betes ... Dia dia ... Dia leptin ... Dia leptin ... Leptin Leptin ... Dia dia ...

Comments
I chuckled, a little.
You don't think getting an MD adds to this ability at all? I'm surprised, but then I only have a vague idea of what goes on in doctor school. From what I've been able to gather it seems to involve lots of memorization and dead bodies. Otherwise I'm not really sure what they do... so maybe you're right.
But seriously, unless you are an insurance underwriter, why quibble about the precise curve that is fit to the Batty et al. data, or even the normalization of the blood glucose values? The sense of the result is pretty clear: when you walk into a lab for a 50g glucose challenge, you don't want your blood glucose to be wildly elevated after two hours. And if you are an underwriter, the Batty et al. data could be massaged into a pretty decent predictor.
But as far as I could tell from a cursory read of the paper, the Batty et al. results do not say anything about the relationship between typical postprandial blood glucose values and anything at all. Batty et al. is just a correlation between outcomes and the result of a glucose challenge to otherwise healthy men.
I wonder if there is a dietary strategy that will improve your response to a glucose challenge? I seem to recall reading someplace that there was an opposing strategy that is practically guaranteed to yield poor results to a glucose challenge ...
PS: No serious scientist would fit un-motivated curves to the tree data and call it modeling. Just fitting polynomials to data and using the resulting curve for anything at all is a story kind of like chi-by-eye, but the kung fu ending in that case is the poor slub being wacked in the back of the head by everybody that walks by. So when it must be done, be sure to make a grad student do it.
I just read the same here:http://www.sciencedaily.com/releases/2011/12/111208184651.htm
"An intermittent, low-carbohydrate diet was superior to a standard, daily calorie-restricted diet for reducing weight and lowering blood levels of insulin, a cancer-promoting hormone, according to recent findings."
And being fair, insulin has pro-carcinogenic effects...
I think you mean that hyperinsulinemia due to insulin resistance has pro-carcinogenic effects.
I think it's a mistake to equate this with normal, healthy insulin levels having pro-carcinogenic effects.
@David: Welcome! Well, that is certainly true and the inside-outside joke of PhD standing for piled higher and deeper has persisted because it has a kernel of truth to it. By no means am I saying that every scientist is above criticism either. But the vast majority of PhD's are not idiots with no clue how things work in the "real world".
I'm not sure how to take your last comment. I did a quick Google image search for an exponential which is how I found that page. Was looking for a bit more scatter in a plot to make a point. That point being that a linear fit can be adequate to describe something but not necessarily representative of what's going on. I'm not saying anything about trees ;)
So my choices are diabetes or cancer? Shucks...
Just kidding. I was really more fascinated at the idea that a group of people who have been upset at the way cholesterol is unfairly demonized as promoting heart disease and given silly prefixes like "artery clogging" turn around and describe insulin as a factor in cancer progression.
I think it's another facet of the same double standard that leads them to dismiss scientists and researchers on the one hand, then dismiss others for lacking credentials on the other. You start to get the impression that the favorite cheat food for many LCers is the pretzel.
To call insulin a pro-carcinogenic hormone is irresponsible in my opinion. It's like other growth factors and hormones being labeled as such. That's why children are so cancer ridden I suppose. :(
I'm so sick of the consequences hyperinsulinemia/IR being conflated with normal postprandial insulin spikes.
http://cancerprevention.aacrjournals.org/content/2/8/720.full
I think it's a stretch for anyone to go from insulin levels being a biomarker for breast cancer to calling insulin a cancer-promoting hormone. Sigh.
http://www.youtube.com/watch?v=VKs0oEIVOck
That insulin is pro-carcinogenic doesnt means that raising insulin to normal levels causes cancer. That is stretching the truth. Im just saying that insulin, as a growth factor, can promote and aggraviate cancer in the appropiate conditions.
@Evelyn,
Cancer cells have defects in cell cycle progression check points, as well as in apoptosis and growth control. One of the most common pathways dysregulated is the IR/IGF-1/IRS/PI3K/Akt/mTOR pathway, which promotes cell growth, and inhibit pro-apoptotic factors, activating anti-apoptotic factors. Other growth factors acting through the Ras-Raf-MEK-ERK pathway also contribute to carcinogenesis. Any growth factor can contribute to carcinogenesis (see for example, CIVAMAX-EGF for lung cancer, the new Ab vaccine). This is not controversial at all.
"That's why children are so cancer ridden I suppose. :("
Children need growth factors in order to grow (!). However, any excess of growth factors can contribute to cancer risk.
There are A TON of studies done in vitro and in vivo demonstrating the carcinogenic role of insulin. You can search them if you want. This is why insulin (as well as leptin) is a marker for cancer risk.
Im not saying that insulin per se is enough to cause cancer, so please dont think that I follow the carbohydrates-->insulin-->cancer logic. However, any excess of growth factors can contribute to carcinogenesis, so IMO it is important to have normal/low levels of plasma growth factors (insulin, IGF-1, etc.). If you have already developed cancer, this is more important.
My main point was that a response to a glucose challenge test is not really relevant to a discussion about desirable postprandial blood glucose levels unless your typical meal is a solution with 50g glucose and nothing else. Many people would see improved responses to a glucose challenge with a higher carb diet, even if such a diet results in much worse postprandial values. Since very low carb diets are well known to result in poor responses to glucose challenges (unless your cheat by carbing up for a few days, but if you're going to game the test what's the point of taking it?) I'm arguing that the Batty results are actually pretty good evidence against recommending a very low carb diet.
I'm not arguing that high postprandial blood glucose values are desireable: only that the Batty paper does not by itself argue against them. I'm generally of the opinion that modifying your behavior to get a low risk on some arbitrary predictor probably destroys the value of the predictor ... but if you otherwise wanted to follow a lowish carb diet and still fall into a good risk column in the Batty table, some safe starches are probably a pretty good way to go (regardless of the normalization of the blood glucose values).
The last part of my last comment was primarily a response to the recent discussions about how 'serious' scientists behave. It's not entirely relevant, but here is a quick clarification. When fitting data, you typically find yourself in one of a few situations. If you have lots of data, then great! Don't fit anything: respect the data and use non-parametric techniques. On the other hand, perhaps you have a great physically motivated model but not very good data. In that case, knock yourself our and determine the model parameters as best you can from the data you have. Generally, the only time you are tempted to fit a polynomial (or a linear threshold), is when you don't really have good data, and you also do not have a well motivated model. In this case it's almost always a bad idea to proceed.
In the case of the Batty table, you can adequately fit a linear threshold model, but as soon as you do so you begin to constrain your thinking on the topic, so the model should be well motivated. Better to just let the data speak for itself. Of course, a 'serious' scientist would have facilitated this by using logarithmic bins instead of that multi-resolution table :)
Post a Comment
Comment Moderation is ON ... I will NOT be routinely reviewing or publishing comments at this time..