More on Look AHEAD
Thanks to the many readers who supplied links and additional information in comments on my last post on that diabetes study run amok (grin).
Phase I = First Year: Lifestyle Intervention [subjects] will be seen four times per month (three group sessions and one individualized session) for six months and then twice per month for six months, with an opportunity for more frequent follow-up. The goal will be to induce a 7-10% weight loss and to increase exercise to 175 minutes per week. Participants assigned to Diabetes Support and Education will be offered three educational/support sessions.
Only the first year was intended to be a weight loss phase.
Phase II Years 2 thru 4: Lifestyle Intervention [subjects] will be seen at least one time per month in person with at least one other contact each month (in person or by phone, e-mail, voice-mail, or mail). The goal of Phase II is to maintain a weight loss of 7-10% and an activity level of greater than 175 minutes per week. Participants assigned to Diabetes Support and Education will be offered three educational/ support group sessions each year throughout this phase. Assessment will occur by phone every six months and at annual clinic visits.
And now from the 4 year followup, how did Phase II go? (ILI = dieters, DSE = control)Phase III Years 5 and beyond: ...the primary purpose being to follow participants for the monitoring of cardiovascular events. Since participants are recruited over 2.5 years, this phase of the trial will be variable length, ranging up to 13.5 years. Participants in the Lifestyle Intervention will be offered monthly on-site individual contact with a counselor. Open groups will be offered one time per month. Sites will offer one refresher group and one national campaign per year. Participants assigned to Diabetes Support and Education will be seen once yearly throughout this phase, with the added options of continuing to attend one annual session throughout Phase III and repeat the 3 educational sessions for as long as these are being conducted for participants still in Phase II.
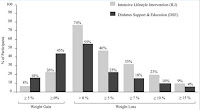
- Average weight loss: ILI: 4.7 ± 0.2% DSE: 1.1 ± 0.2%
- Weight losses were significantly greater in the ILI than the DSE group at all four annual assessments.
- 35% of ILI and 18% of DSE participants achieved the study-wide goal of losing ≥ 7% of initial weight
- 23% of ILI and 10% of DSE participants lost ≥ 10%
- A significantly greater percentage of ILI than DSE participants met each of the categorical weight losses
- Significantly more DSE than ILI participants (45% vs 26%) had gained above their baseline weight at year 4
Here are the graphical summaries of the weight losses (and gains), you can click to enlarge.
Folks, I ask, why even bother with Phase III?? Only around one-third of the dieters had achieved the piddly goal of losing and maintaining more than 7% of their initial body weight, while roughly one-quarter had gained weight above baseline at the end of Phase II. Meanwhile, a significant number of the control group (roughly half as many as the dieters) met the goal of 7% loss, and it is not insignificant that 10% of the control group lost more than 10% of their initial body weight. Bottom line, further follow-up wasn't even testing whether losing 7+ percent of one's body weight would reduce CVD risk. And it's complicated by the fact that significant numbers gained weight.
This study is a royal waste of time and money if all they are going to do is between group comparisons. The differences may reach statistical significance, but when you are an obese person, losing 5% of your body weight -- which only half the dieters even managed to maintain by year 4 (less than half way through the 11.5 year study duration) -- is simply NOT significant. We're talking a 300 lb person losing 15 lbs and still weighing 285 lbs, or a 200 lb person losing 10 lbs and still weighing 190. Hopefully they'll do an additional analysis of weight change vs. outcomes so it's not a total flush of money down the toilet.
It does not surprise me that in shorter term studies we still see some improvements with nominal losses -- it's likely a hang-over of the extended energy deficit. On average, the ISI group was gaining weight in years 2 through 4, and I'm willing to wager that by year 8 even more will have gained back. According to the 4-year paper, those who didn't meet the 7% goal in year 1 were encouraged to shoot for it in year 2 and beyond, but the weight changes say otherwise. And don't give me that eat less/move more doesn't work. Remember Ebbeling et.al.? That was only an "eat less" weight loss study, where the average 230 lb participants lost an average of 15% of their initial body weight in 12 weeks and then maintained that weight for a period of roughly four months by ... eating less than they did before the study. Thus a large percentage of the participants in Look AHEAD are simply not complying with the "intensive intervention".
On one bright note, the group that was at least attempting a more directed intervention fared better in the weight gain department. Roughly half of the DSE group gained some weight and almost one in five gained more than 5% of their initial weight. The ELMMers were half as likely to suffer the same fate. The other bright note is that -- although we don't have many details -- the ELMMers were able to use fewer medications to manage their diabetes. I would say that this alone is encouraging -- even half-hearted ELMMing can improve one's damaged metabolism. Still, I'll hold off getting too excited about this until there's more information. My bet would be on those losing the most weight were the ones able to reduce/eliminate meds, or perhaps they MMed enough to improve insulin sensitivity even in the absence of good adherence to dietary prescriptions and weight loss.
One last thing as regards the benefits of nominal weight losses. I'm not sure if it's wishful thinking, misplaced enthusiasm from short term results, lowering expectations or some combination of it all. As I stated earlier, my gut feeling is that many of the shorter term studies out there are still looking at "hang-over effects" from the chronic caloric deficit phase. It seems quite encouraging to be able to tell a 250 lb diabetic that even losing 15 lbs can produce dramatic improvements, but I doubt this will be a lasting effect once the person has stabilized out at 235 lbs, because the fact of the matter is that the caloric intake to sustain that weight is in excess of homeostasis for a normal weight ... and to borrow a phrase from the slicker science guy, will clog the metabolic works.

Comments
The reason Look AHEAD was terminated early is that it was hopelessly underpowered. The event rate was nearly 4X lower than expected. It's still possible that the intervention would have been highly successful, but we'll never know because the study design turned out to be inadequate. Still, they found improvements in several secondary endpoints.
http://www.drsharma.ca/looking-back-at-look-ahead.html
I'll wait for the final analyses which hopefully will break down the data by those who achieved the weight loss goal of >7% and maintained it. Since they are looking at just nominal weight loss, they really should exclude those who lost more than 10% and/or break that data out as well.
A weight stable obese person can be in cellular excess. Most obese have higher muscle cell triglyceride content than lean.
This discusses how Mexican-Americans are more prone to diabetes because of fat around the pancreas.
http://www.sciencedaily.com/releases/2012/09/120911102948.htm
ProudDaddy's latest postulation is that it also makes a difference whether you are losing or gaining weight.
I'll effort the full text, but this is fascinating.
Post a Comment
Comment Moderation is ON ... I will NOT be routinely reviewing or publishing comments at this time..