A tale of two "Wheat Bellies"
Before Dr. William Davis' name became synonymous with the elusive* Wheat Belly, he was well known for his subscription Track Your Plaque website. This website currently charges $90 (all prices rounded) for the first year with yearly renewals at $72, for the basic membership ... more for shorter "contracts". That's just the membership fee, that basically affords you discounts on various TYP products such as your Basic Membership Kit for $70 (reg. $110) or a Supplement Kit for $175 (reg. $215) or the testing kit for a cool $530 (reg. $570). In the marketplace you can purchase all manner of testing supplies, etc.
Now Davis is a huge backer of Jimmy Moore's Cholesterol Clarity book. He contributed to it as an expert, provided an Editorial Review for Amazon.com and, as if that weren't enough, offered up a glowing 5 Star review on same, entitled Cholesterol bashing at its finest. In it he writes:
Uninfluenced by them, but influenced by profiteers and profiteers in their own right nonetheless.Widely-held beliefs, many of them propagated by "official" agencies like the FDA, USDA, American Heart Association, Academy of Dietetics and Nutrition, American Diabetes Association, etc., are crumbling under the scrutiny of informed people uninfluenced by the pharmaceutical industry, agribusiness, or the excessive profiteering ways of modern "healthcare."
In Cholesterol Clarity, Jimmy Moore, along with the help of a couple of dozen other vocal critics of the Lipid Hypothesis, systematically take apart the flawed logic often used to justify a $23 billion per year statin drug industry. He exposes the overly-simplistic thinking and the "research" used to prop up this example of how far wrong medical care can go when richly funded. Jimmy shows how the fiction that "cholesterol causes heart disease" belongs with other fairy tales like "Cut your fat and saturated fat for heart health" and "Fat makes you fat."
Actually, while there is an undercurrent about diet and low fat diets, this book really does none of what he claims. He did, however, get the anti-industry statin bashing correct.
We live in a time when the messages in health have been distorted by bad science and biases introduced by corporate interests that stand to gain from a campaign of half-truths. In his characteristically genuine and straightforward style, Jimmy helps the reader understand how to navigate the real arguments behind heart disease risk unemcumbered by self-serving financial interests.
Oh the irony. Nuff said. The general take-aways from the book are that nobody should be on statins, lowering cholesterol levels is misguided and will harm you, and LDL-C and even LDL-P are totally irrelevant if you have good HDL-C, low small LDL-P, low trigs and/or your LDL particles are the fun-loving, life-giving "large and fluffy" kind.
One would think that Davis promotes this approach on TYP, right? That you shouldn't be at all concerned over elevated cholesterol? Wrong. Here is a 2006 publication from TYP: TYP Special Report: Unique nutritional strategies to reduce cholesterol naturally (ht C.Grashow) . But, but ... perhaps he has changed his tune? Nope: Health Diagnostics Lab Explained -- 8/15/2013.
Low-Density Lipoprotein (LDL) is composed of phospholipids, triglycerides, cholesterol, and a Apolipoprotein B (ApoB).
There is a 2-3x increased risk of cardiovascular disease when LDL-c, ApoB, and LDL-P are all 3 elevated.
Goal – < 100 mg/dL or < 70 mg/dL if there are other risk factors for heart disease or diabetes. Notice that this is a measurement of weight. It is measured in mg per dL. It does not tell us the size of the LDL particle or the number of LDL particles.
What to do to improve it – The first intervention is to improve overall health through the ‘Healthy Trinity’. We recommend RevChol if we cannot reach our goal.
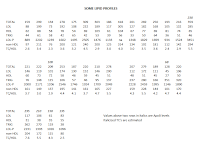 I would note that RevChol is a pharmaceutical grade O3 supplement, so much for consistency on the pharmaceutical industry. But note the recommendation to lower LDL-C. He has not changed in his marketed-to-the-mainstream message, which means the sugary (excuse me, sucralosely) words for Jimmy Moore are knowingly targeted at the true believers. And I'd dare say (click to enlarge) he'd take issue with the majority of the lipid profiles in the top "row" here that Jimmy Moore designated as "healthy" in his book -- especially that one in the top right from guess who.
I would note that RevChol is a pharmaceutical grade O3 supplement, so much for consistency on the pharmaceutical industry. But note the recommendation to lower LDL-C. He has not changed in his marketed-to-the-mainstream message, which means the sugary (excuse me, sucralosely) words for Jimmy Moore are knowingly targeted at the true believers. And I'd dare say (click to enlarge) he'd take issue with the majority of the lipid profiles in the top "row" here that Jimmy Moore designated as "healthy" in his book -- especially that one in the top right from guess who.
Davis focuses on the small LDL particles in some of his MOC's (Moment of Clarity, what Jimmy designates his quotes). So the question is, does he really have two standards? Does he believe in the benign large fluffy LDL? Because none of this comes of anywhere near as forthrightly as it does in the book.
“Of the thousands and thousands of patients I have personally seen over the years with coronary disease, I can count the number of people who lacked a prevalence of small LDL particles on one hand. It is possible for it to happen, but it’s highly unusual. The vast majority of people who have coronary disease or a risk of developing it have an excess of small LDL particles. There’s only one thing that causes small LDL particles and that’s carbohydrates, not dietary fat. We use a low-carb diet to eliminate the expression of small LDL, which also, by the way, reduces blood sugar levels and normalizes blood vitamin D levels.”
Which wouldn't be quite so bad if he were more deferential to other physicians who try to treat their patients to achieve the same goals he claims to promote in his made-for-general-public consumption materials. But no ...
“Sadly, we can’t always rely on our doctors for straight talk and intelligent, insightful answers. As a result, it’s becoming incumbent upon patients to educate themselves, engage with others online who are providing information about nutrition and health, and go into the doctor’s office as empowered patients. Doctors do help every once in a while, but they usually just hand patients some silly prescription.”
I used to read links to TYP that were occasionally posted on Jimmy's forum. They mostly seemed reasonable, though looking back there were signs. However once he got the book deal for Wheat Belly, his writings noticeably changed. He ratcheted up the LC dogma, and of course wheat caused all ills. I put the "*" in my opening paragraph because for all the wheat and gluten bashing rhetoric in the book and blog and other writings and speeches, Davis has failed miserably in the prime objective of titling a book as he did: He never provides any evidence that wheat in particular is responsible for obesity, and especially abdominal obesity. Fail.
But here's an interesting thing from the 2006 link -- I feel the need to note that I'm not making this stuff up here!
Beta-glucan is a soluble fiber that avidly absorbs water and transforms into a gooey gel. This gel, as it traverses the twenty-some feet of intestine, is an efficient absorber of cholesterol. Beta-glucan is responsible for the cholesterol-lowering properties of oatmeal. You know what’s even better than oatmeal? Oat bran. You can buy oat bran in bags and boxes in most grocery stores. Oat bran is also more versatile. You can use it as a hot cereal microwaved in skim milk or soy milk (add raw sunflower or pumpkin seeds, fresh berries, or sliced fruit), or you can add it to yogurt, fruit smoothies, or protein drinks. One ounce of uncooked oat bran (1/4 cup) contains 4 grams of fiber, of which 3 grams are soluble. Including ¼ cup of oat bran a day in your diet can powerfully reduce cholesterol.
 I don't think I need to remind my regular readers about Davis' newfound obsession with the evils of oatmeal. A small bowl will send your blood sugar through the roof, and don't get any in your eye lest you burn your corneas with sulfuric acid. In my post entitled Wheat Belly on Acid, I discussed this nonsense where oats topped a list of sulfuric acid containing foods. When did he learn this? Below are screenshots from nutritiondata.com for 100g (a little over a cup, uncooked) oats vs. oat bran (links are in images).
I don't think I need to remind my regular readers about Davis' newfound obsession with the evils of oatmeal. A small bowl will send your blood sugar through the roof, and don't get any in your eye lest you burn your corneas with sulfuric acid. In my post entitled Wheat Belly on Acid, I discussed this nonsense where oats topped a list of sulfuric acid containing foods. When did he learn this? Below are screenshots from nutritiondata.com for 100g (a little over a cup, uncooked) oats vs. oat bran (links are in images).
You have the same amount of protein (that battery acid making stuff) in each, and an increase from 11g to 15g of fiber seems hardly significant. Further, the "net carbs" are 55g for oat bran vs. 51g for oats. Oh, but perhaps he didn't notice the blood sugar effects of all that glucose spiking?? Nope:
Create a smorgasbord of cholesterol-reducing foods and supplements
Including just a little of one or two of these strategies will help reduce your cholesterol. But if you’re looking for super-charged LDL cholesterol reduction, combine several of these functional foods and supplements. It is entirely possible to reduce LDL cholesterol 30% or more when you put several together each and every day. Here’s a sample approach:
• Raw almonds—½ cup per day (total fiber 5.8 g; soluble 0.6 g)• Oat bran—¼ cup per day (total fiber 4 g, 3 g soluble)• Psyllium seed—2 tsp per day (6 g total fiber; 4.8 g soluble)• Citrus fruit—e.g., 1 orange (around 1 g soluble fiber)• Beans—1/2 cup per day, cooked (4 g total fiber; 1 g soluble)• Soy protein powder—3 tbsp in protein shake (25 grams protein)• Theaflavin—600–900 mg/day; or 6–7 cups green tea per day
The fiber content of this regimen alone—over 20 grams added—packs a powerful effect on cholesterol. Most people lose a modest quantity of weight, as well, because of the feeling of fullness that fiber-rich foods provide and the weight loss effect of green tea. If you are diabetic or have “borderline” or “pre-” diabetes, blood sugars are often LOWER {emphasis mine} on this regimen. (Discuss this with your doctor to avoid excessively low blood sugars if you take oral diabetic medications or insulin.)
Yes ... William Davis is a pretty common name, so reading such might make one wonder if we're talking about the same guy. We are. But now (Oct 2011 actually)
Wheat Belly: Quick and Dirty
This is the very same diet I advise for patients in my office that achieves spectacular reductions in small LDL particles (the #1 cause of heart disease in the U.S), as well as unraveling diabetic/pre-diabetic tendencies. The diet starts with the biggest step: elimination of wheat. But a healthy diet cannot end there, else you and I could eat no wheat but fill our calories with soft drinks and jelly beans. So the next step is to limit carbohydrates if your goal is to lose more weight and correct metabolic distortions like high blood sugar and small LDL particles.
Eliminate:All wheat-based products (all breads, all breakfast cereals, noodles, pasta, bagels, muffins, pancakes, waffles, donuts, pretzels, crackers), oat products (oatmeal, oat bran), cornstarch-based products (sauces or gravies thickened with cornstarch, prepared or processed foods containing cornstarch, cornmeal products like chips, tacos, tortillas), sugary soft drinks, candies
I don't need to quote the whole thing. Nuts and seeds are still OK, but other items from the cholesterol lowering list -- legumes and fruit (citrus) -- are now also to be limited.
Lastly, Davis is very anti-statin. OK. But in the one clinical trial he participated in, guess what? You got it. Statins were used: Effect of a Combined Therapeutic Approach of Intensive Lipid Management, Omega-3 Fatty Acid Supplementation, and Increased Serum 25 (OH) Vitamin D on Coronary Calcium Scores in Asymptomatic Adults (ht CG again)
Abstract
The impact of intensive lipid management, omega-3 fatty acid, and vitamin D3 supplementation on atherosclerotic plaque was assessed through serial computed tomography coronary calcium scoring (CCS).
Low-density lipoprotein cholesterol reduction with statin therapy has not been shown to reduce or slow progression of serial CCS in several recent studies, casting doubt on the usefulness of this approach for tracking atherosclerotic progression. In an open-label study, 45 male and female subjects with CCS of ≥ 50 without symptoms of heart disease were treated with statin therapy, niacin, and omega-3 fatty acid supplementation to achieve low-density lipoprotein cholesterol and triglycerides ≤60 mg/dL; high-density lipoprotein ≥60 mg/dL; and vitamin D3 supplementation to achieve serum levels of ≥50 ng/mL 25(OH) vitamin D, in addition to diet advice.
Lipid profiles of subjects were significantly changed as follows: total cholesterol −24%, low-density lipoprotein −41%; triglycerides −42%, high-density lipoprotein +19%, and mean serum 25(OH) vitamin D levels +83%.
After a mean of 18 months, 20 subjects experienced decrease in CCS with mean change of −14.5% (range 0% to −64%); 22 subjects experienced no change or slow annual rate of CCS increase of +12% (range 1%-29%). Only 3 subjects experienced annual CCS progressionexceeding 29% (44%-71%). Despite wide variation in response, substantial reduction of CCS was achieved in 44% of subjects and slowed plaque growth in 49% of the subjects applying a broad treatment program.
So there you have it. As they used to say at the end of the old game show: Would the real William Davis MD please stand up!


Comments
KH: What got you interested in studying the combination therapy of a statin drug, niacin, omega-3 fatty acids, diet and vitamin D supplementation in asymptomatic adults?
WD: The program that was described in the published study came about incrementally as part of my efforts to achieve reductions in CT heart scan scores. Heart scan scores, or “calcium scores,” provide an index of the quantity of atherosclerotic plaque in the coronary arteries. They quantify plaque and provide an index that can be tracked over time to assess the success or failure of various preventive efforts. Several studies have demonstrated that, without preventive efforts, calcium scores can be expected to increase between 15-40% per year. We learned a number of years ago (unpublished data)
that obtaining conventional lipid values of LDL cholesterol 60 mg/dl or less, HDL cholesterol 60 mg/dl or greater, and triglycerides 60 mg/dl or less (60-60-60) was associated with increased likelihood of arresting the increase or reducing heart scan scores. Thus, several of the strategies employed targeted the 60-60-60 lipid values. Accordingly, the lipid values in the study showed dramatic changes: total cholesterol
was reduced by 24%, LDL was reduced by 41%; TG were reduced by 42% an HDL levels were increased by 19%.
KH: What exactly was the diet therapy? What was the major goal of the diet? To reduce inflammation? Lower lipids? Etc.?
WD: Participants were counseled on the American Heart Association Step II diet with 30% of calories from fat, =7% from saturated fat. (Interestingly, more recently, though not reflected in this study, we have used a low carbohydrate diet that restricts wheat, cornstarch, and sugar and preliminary results suggest improved results).
KH: Who is a candidate for your program? How would you use this information clinically?
WD: Candidates for the clinical program include anyone with a heart scan score (coronary calcium score) above zero, indicating long-term risk for heart attack and development of heart disease. Despite the fact that coronary heart disease is the number killer of American men and women, we have no readily available tracking strategy to follow the course of this disease with ease and precision. Standard testing techniques such as EKGs, stress tests, and cholesterol panels can not be used to precisely track the course of coronary disease. A heart scan that yields a coronary calcium score can conceivably be used as a tracking mechanism to gauge progression, stabilization, or regression.
-
Abstract
Tracking of coronaryartery calcium (CAC) has been suggested for monitoring the effects of lipid control, but it is not known whether lipid control decreases progression of CAC. Seven hundred sixty-one subjects (mean age 64.5 ± 7.3 years; 91% men; 69% positive for CAC) in an ongoing cohort study underwent baseline and follow-up (after 7.0 ± 0.5 years) computed tomography for CAC. Subjects were stratified into low-risk (<2 risk factors), intermediate-risk (≥2 risk factors but <20% risk of coronary heart disease over 10 years), or high-risk (≥2 risk factors and >20% risk of coronary heart disease in 10 years or diabetes) groups. Lipid control was defined according to criteria of the National
Cholesterol Education Program. Two-way analysis of covariance was used to examine the relation of low-density lipoprotein (LDL) cholesterol and risk group to change in CAC volume score. Control of levels of high-density lipoprotein (HDL) cholesterol and triglycerides was also examined in relation to progression of CAC. After adjustment for other risk factors and baseline CAC volume, CAC progression was similar between those with adequate and those with inadequate control of LDL cholesterol (p = 0.68) and across categories of optimal, intermediate, and higher risk LDL cholesterol (p = 0.40). However, higher levels of HDL cholesterol (≥1.5 mmol/L [60 mg/dl]) were associated with less progression of CAC volume (151 vs 203 mm3 in those with HDL cholesterol <1.0 mmol/L [40 mg/dl], p = 0.03). There was no relation between triglycerides and CAC progression (p = 0.54). Our findings do not support the use of CAC assessment for monitoring the control of LDL cholesterol, but greater progression of CAC may occur in those in whom HDL cholesterol is not controlled.
SO - why is wheat belly basing EVERYTHING on CAC??
http://blog.trackyourplaque.com/2010/10/butter-just-because-its-low-carb-doesnt-mean-its-good.html
So there’s nothing wrong with the fat of butter. It’s AGEs that appear to be responsible for the endothelial dysfunction/artery-constricting, insulin-blocking, oxidation and inflammation reactions that are triggered. Among all of our food choices, butter is among the worst from
this viewpoint.
Throw in the peculiar “insulinotrophic” effect of butter, and you have potent distortion of metabolic pathways, courtesy of the butter on your lobster.
OMG - NO BUTTER
The ONLY medical personne reallyl interested in "cholesterol' are GPs. this is because they are constantly exposed to Big Pharma marketing. Cardiologists on the other hand are generally quite nonchalant about "cholesterol" and far more concerned with the REAL risk factors - hypertension, besity smoking, metabolic disease and lack of exercise. [Two of my siblings are ex smokers. Both have had minor infarcts. Neither was placed on statins by their respective cardiologists.]
The NHBLI questionairre gave me a trvial 1% probability of an infarct in the next 10 years even when I entered trageously high "cholestrol" values. This is because don't smoke, have a low BMI, no diabtes, low blood pressure (95//70) and am physically active.
http://cvdrisk.nhlbi.nih.gov/calculator.asp
Helping others ... I am still amused by how many think Mark Sisson's blog exists for that reason. He was very forthright (shockingly so considering who he was talking to) about it's purpose in our phone conversation: to sell supplements and books.
I do remember this post ... it was discussed on Jimmy's forum. So devoted are the low carbers, however, they dismissed this info because everyone has a bad day.
What would be funny, but probably not worth my time, would be a Battle of the Cholesterol Clarity Experts series. Masterjohn vs. WB on butter! Chis for FTW!!
FWIW, there's a lot of exaggeration going on as to the statin-pushing doctors here. For one, they don't make a red cent off of prescribing them and the generics are quite cheap these days. Which is not to say some docs don't do it (and it's more the insurance companies behind it now :( ) but most will not look askance at mildly elevated lipids.
Re: obesity and metabolic disease (diabetes/IR I presume?) -- lipid derangement tends to precede and forewarn of these issues.
MOST people who have fatal heart attacks have NORMAL cholesterol levels.
Directly manipulating cholesterol levels by medication has NO effect on mortality.
Statins are believed to have a secondary anti-inflammatory mechanism which is responsible for any reduction in mortality.
At best blood lipids are an indication of an unhealthy lifestyle. At worst they are a totally meaningless distraction.
Current medical research strongly suggests that atherosclerosis is the end result of chronic oxidative stress due to poor diet and a lack of exercise. In this case elevated LDL is may be a symptom of heart disease not a cause.
Medicine is a skilled trade not a science. It is primarily concerned with treating SYMPTOMS rather than underlying disease processes. This is a relic of the mostly false "Silver Bullet" theory which assumes that a) any disease process can be successfully treated by medication and b) successfully treating the symptoms cures the disease.
Uncovering a Hidden Source of Cardiovascular Disease Risk
By William Davis, MD
"Saturated fats, like those found in butter, shortening, and fried foods, are especially potent inducers of excess postprandial lipoproteins. Because postprandial disorders cause fats to linger longer, avoiding unhealthy fats is doubly important. Minimizing these fats is advisable for other reasons, such as reducing LDL, blood pressure, inflammation, and cancer risk. While avoiding saturated fats will not eliminate postprandial lipoproteins, it will help reduce them
The following strategies can reduce triglycerides dramatically, and help reduce or eliminate IDL and postprandial lipoproteins:
Soy protein (20 grams per day) from tofu, soy milk, soy protein powder, and other sources can lower LDL by 10-20 mg/dL and reduce postprandial lipoproteins by 10%.
Statin drugs such as Zocor®, Crestor®, and Lipitor® not only lower cholesterol, but can reduce postprandial lipoproteins by 30-80%.
Fibrates (cholesterol-lowering drugs such as Lopid® and Lofibra®) can reduce postprandial lipoproteins by 70%. They can be a useful second-line strategy if fish oil, weight loss, and nutritional efforts fail to do the job."
One of my readers sent me an e-mail with concerns about the diet you recommend in “Track Your Plaque” because it is basically a lower-fat approach (albeit, not as low-fat as Dr. Ornish recommends). Your diet calls for 24 percent fat coming from unsaturated fat sources in conjunction with a high-fiber (35g daily) intake. What are your thoughts about a higher fat diet and more specifically one that includes saturated fat?
The Track Your Plaque book was written in 2003 before its publication in 2004. Much has happened in the few short years since its release.
Among the changes to the somewhat low-fat approach articulated in the book is diet that has proven more effective in correcting the causes of heart disease: a diet higher and
richer in healthy fats like those from fish, raw nuts, olive oil, canola oil, flaxseed and grapeseed oils, and wild game. These changes, along with a reduction in carbohydrate content, suggest that a diet that is at least 30% fat (calorie percent) is probably more towards the ideal.
However, I do believe that saturated fat remains an issue. Saturated fat really became an issue when humans began to fry their foods and add animal fats like butter and shortening. It became an even bigger issue when the “factory farm” phenomenon seized control of American farming away from the traditional family farm, introducing economies of scale like corn feeding of livestock that transformed beef, pork, and chicken into high saturated fat foods.
The trend to reject saturated fat is really a trend towards rejecting the factory farm movement drivenby enormous multi-national corporations intent on supporting the fast
food and processed food industries.
I lost nearly 200 pounds on the Atkins diet back in 2004 and have been able to maintain that weight loss ever since by continuing to implement the principles I learned from the late great Dr. Robert C. Atkins. And yet you do not recommend this particular way of eating overthe long-term as a way to improve health. What specifically is unhealthy about eating an Atkins-styled diet beyond weight loss and is there a better way of eating that you believe is both heart healthy and bring about weight control?
Interestingly, before Dr. Atkins died, he articulated a diet that was more balanced in monounsaturated fats, less rich in saturated fats, included more vegetables, fruits, nuts, and other healthy foods.
We need to remember that the “Induction phase” of the Atkins’ diet that permitted unlimited intake of meat, cheese, and other saturated fat-rich foods was simply that—-the induction into the world that allowed you to be divorced from the addictive property of refined carbohydrates.
In we were to follow the Induction phase of the Atkins’ diet
indefinitely, we would experience increased bladder infections, kidney
stones, rashes, osteoporosis, cancer (liver, colon, prostate, breast),
diverticulosis, and other chronic conditions. The induction phase is a
useful tool to make the break from carbohydrate-addicted physiology, but
not a recipe for long-term health.
My blood pressure is lower, my HDL higher.
He is certainly on to something, and is not anti-statin, just suggests other routes to heart health. Oh yes- my cholesterol is and has been in the 200's. I am thankful for Dr Davis.
http://medres.med.ucla.edu/Research/posters/Amit%20Sachdeva%20-%20Lipid%20Levels%20in%20Hospitalized%20Pts%20with%20CAD.pdf
LDL 70-100=11.7%, LDL 100-130=10.6%
HDL ≥ 60 +
LDL <70 = 1.4%, LDL 70-100 = 2.5%, LDL 100-130 = 2.1%
I developed severe hypercholesterolemia on an Atkins diet. Not good.
I use a moderate version of carbohydrate restriction and veganism in my own diet, but do not promulgate as such to my own patients.
I have started eat more grains and am enjoying that, with no weight rebound.
My BP is the lowest it's ever been since I started monitoring it - about 106/78 (first reading in a busy pharmacy). My carb intake is definitely over 100 g per day now.
Statins, cholestyramine, ileal bypass, low fat diets have all been shown to prevent cardiovascular events and all share the common property of lowering LDL cholesterol levels. All are supported by hard evidence randomized trials.
I don't doubt that TYP has helped people. The point of this post is to point out inconsistencies. If you read his reviews of Jimmy Moore's book he comes off very anti-statin and mainstream POV on cholesterol.
The general tone of that book was that high LDL is almost never a problem, except, apparently if you have high small LDL-P or triglycerides in the high normal range. That's pretty far astray from what the scientific evidence supports.
I would also say that fish oil and other supplements may well be more responsible than ditching wheat for which there is absolutely NO evidence linking it to heart disease.
A large meta-regression of more than 100 such trials found that the degree of CV event reduction was directly correlated with the degree of cholesterol-lowering seen in the trials.
STARS randomized to usual care, low fat diet, and low fat diet plus cholestyramine. Therefore, it has unique ability to tease out the effects of both cholestyramine and diet. The combined arm did best.
POSCH has recently reported 25 year data which are impressive.
The statin skeptics need to explain why multiple interventions that directly lower cholesterol reduce the risk of cardiovascular events. They keep resorting to 'pleiotropic effects' but miss the general direction of the evidence base from trials, genetics, observational cohorts, animal data, etc. You may want to check out http://healthylongevity.blogspot.ca/
2) A meta-regresson analysis is observational in nature and can't assess causal relations. The phrase Garbage in, Garbage out applies here and it is not surprising that a pharmaceutical funded analysis would come to that conclusion.
3) There was barely any difference between diet only and combined group in the STARS trial. The intervention groups increased n-3 (double), fruit and vegetable intake and reduced processed food and trans fat intake. They also lost weight. Yea, not surprising they did better.
4) Again, the POSCH trial was as much a weight loss trial as anything else and there is no info whatsoever on the dietary and lifestyle habits of the subjects post 1990 (the end of the formal trial). Not even the author knows. Interestingly these same authors state in their paper of post trial follow ups "The recent reports of observations made after the period of a clinical trial must be viewed with circumspection." In the formal trial itself (9.7 year follow up), there was no statistically significant differences in the primary and secondary endpoints of CHD and overall mortality despite large differences in cholesterol.
5) There is no "general direction". It has been a preponderance of failures that has somehow turned into a "preponderance of evidence". A lot of it stems from the fact that a lot of contradictory data is ignored or interpreted without regarding alternate possibilities. There are tons of animal data showing very large reductions in atherosclerosis in the face of extremely high cholesterol so I'm not sure how that supports your case. Animal data in fact contradicts the idea that cholesterol is a major factor.
I am glad you have found something that is making you healthier and hopefully it continues to work for you.
Now in the grans scheme of science your anecdotal evidence means absolutely nothing. There are a Billion of people in this world who do enjoy their wheat every day. The VAST majority of them are in good health and will enjoy it until a ripe old age. In most population studies high carb consumption, including wheat (med. diet) is associated with greater health and longevity.
If you note the 2013 post, Davis hasn't really changed much. He just tailors one message to one audience and his more hyperbolic one towards another. I have a hard time believing those who say wheat alters their BG more than other refined carbs. How do you do with instant oatmeal for instance? Powdered mashed potatoes? White rice? How about an OGTT? I think it is fair to ask given your proffer of anecdotal evidence.
http://www.ncbi.nlm.nih.gov/pubmed/20129375
http://www.ncbi.nlm.nih.gov/pubmed/8994420
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3374116/
http://www.ncbi.nlm.nih.gov/pubmed/20229247
http://www.ncbi.nlm.nih.gov/pubmed/20203302
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3540845/
http://www.ncbi.nlm.nih.gov/pubmed/22670805
http://www.ncbi.nlm.nih.gov/pubmed/21920771
To ignore this is to put one's head in the sand (not being ad hominem here).
Yes there have been failures (MRFIT, etc), but the fact is that dropping cholesterol substantively by diet or drugs typically prevents cardiovascular events. I don't think any mainstream scientists or physicians currently dispute this, regardless of what you might read from internet blogs. Why do you think Big Pharma is pursuing the next biggest cholesterol-dropping drugs (PCKS9 inhibitors)? If they don't work, and there is no track record to suggest that cholesterol reduction does anything, why would they be spending billions of dollars to try and develop a new drug that reduces cholesterol, testing it according to FDA standards to prevent cardiovascular events (by the way, I could have also mentioned SHARP with simvastatin-ezetimibe).
And a total FASTING (let alone postprandial) cholesterol of over 300 mg/dl on an Atkins diet is extremely dangerous. Patients with cholesterols that high had a 7-fold increased risk of dying from coronary disease in Framingham compared to patients with more 'reasonable' cholesterol levels.
In the JUPITER trial, patients whose LDL cholesterols were less than 50 mg/dl had the lowest rates of mortality and cardiovascular events (compared with all other subgroups defined by lipid or lipoprotein status). Could be healthy adherer effect, but it is consistent with the rest of the literature. You might want to check out a book called 'The Cholesterol Wars' by Daniel Steinberg, a biochemist at UCSD. Thank you.
When Esselstyn and Ornish conducts an RCT comparing their diets to others (Atkins, Mediterranean etc.) on mortality outcomes then I will take notice. Their claims are full of hot air.
2) As far as diet trials go, do you conveniently ignore trials that lowered cholesterol but failed or those that didn't lower cholesterol but succeeded? Lowered cholesterol is not what makes the difference. Actually, successful trials typically involve increasing fruit, vegetable and n-3 fatty acid intake regardless of whether cholesterol is lowered or not.
3) The JUPITER Trial (which was rightly criticized) showed no cardiovascular mortality benefits and the alleged total mortality benefit may have been due to a chance finding of fewer cancer deaths in the intervention group. The possible chance finding was acknowledged by Dr. Ridker himself - http://www.ncbi.nlm.nih.gov/pubmed/19427439.
4) In the SHARP Trial, most of the benefit came from softer endpoints. No difference in CHD mortality or total mortality whatsoever and is unlikely to be explained by being "underpowered" since there wasn't even a trend of benefit with 1 more CHD death and over 20 more overall deaths in the intervention group. Not my definition of "benefit".
5) I do have Steinberg's book and read many of his publications but as with people on both extremes the data is selectively cited/interpreted.
Sure there are interventions which have reduced cholesterol and have not prevented cardiovascular events - does that invalidate the cholesterol hypothesis? Hardly. Some of the interventions had major off-target toxicity - e.g. probucol, CETP inhibitors, clofibrate. If high-risk patients in trials are dropping dead from non-cholesterol related drug-induced events there is less chance to reduce their risk of dying from a (modifiable) cholesterol-related atherosclerotic cardiovascular disease burden.
I have not even cited the entire database of interventions that have lowered cholesterol and reduced cardiovascular events - we did not discuss the Air Force Regression Trial (which used 4 non-statin lipid-lowering drugs) or the Stockholm Trial (which also used non-statin lipid-lowering drugs). Nor did we discuss the gemfibrozil trials, bezafibrate (BIP long-term follow-up) or the results of fenofibrate trials (FIELD, ACCORD) where CV events were reduced in discrete subgroups with biochemical evidence of metabolic syndrome. The fibrate trials are unique in that LDL cholesterol is largely unaffected, although type of LDL subspecies do shift favorably.
The level of evidence that cholesterol reduction robustly prevents cardiovascular events and the risk of dying from a cardiovascular event is extremely strong in late 2013 (as it has been for many years). Drug companies are vigorously competing to develop the next hypolipidemic agent BECAUSE THIS APPROACH WORKS (the FDA now requires hard outcomes data, except for very rare diseases like homozygous familial hypercholesterolemia, where people don't tend to make it out of childhood alive -- hmm, funny that, given that cholesterol 'doesn't' cause heart disease).
So whether you look at trials, animal studies, Mendelian randomization genetic analyses, kindred studies, observational cohorts, ecological studies, in vitro data - an enormous body of converging lines of evidence suggest that hypercholesterolemia causes cardiovascular disease. That you may find and cherry-pick a couple of studies that were negative or neutral -- well, any field can give you such outliers. Since all statins in my country are now generic, I expect drug use will climb even further. I look forward to trials validating (or not) the use of Vascepa, ezetimibe, welchol, lovaza and newer investigational agents for modifying lipids). Thank you.
Progression and Regression of Coronary
Calcium Score
William R. Davis1
and Susie W. Rockway2
1 Medical
Director, Milwaukee Heart Scan, Wauwatosa, WI
2 Clinical Nutrition, Rush
University Medical Center, Chicago, IL
ABSTRACT
Serial calcium scoring obtained by CT scanning has been proposed as a means of following progression or regression of coronary atherosclerotic plaque. In an open-label study, we combined pharmaceutical lipid treatment with dietary supplementation in
patients presenting with coronary calcium (Agatston) scores ≥ 50 to test the impact on progression or regression of annual plaque growth as measured by serial coronary calcium scoring in a cohort of 45 men and women. Treatment included statin therapy, niacin, the American Heart Association Therapeutic Lifestyle Changes (TLC) diet, omega-3 fatty acids and vitamin D-3 supplementation at levels to achieve target fasting lipid values of: LDL cholesterol ≤ 60 mg/dl, HDL ≥ 60 mg/dl and triglycerides of 60 ≤ mg/dl and a serum level of 25-OH-vitamin D3 of ≥ 50 ng/ml. All atherogenic lipids were significantly reduced when tested 1 to 2 years after treatment (p<0.001). Total cholesterol dropped by 23%, LDL-c by 37%, TG by 29% while HDL significantly (p<0.001) increased by 18%. Unexpectedly, 21 subjects demonstrated reduced calcium plaque burden as evidenced by a percent decrease in coronary calcium scores (ranges from 0 to –64%), while 21 experienced slowing of progression (mean 12%), defined as less than 30% increase in calcium score (ranges 0.95% to 29%), while only 3 subjects continued to progress at a rate greater than 30%. In conclusion, though wide variation in response following this approach is seen, substantial regression of atherosclerotic coronary plaque using a CT calcium scoring approach is achievable with treatment efforts that extend beyond LDL cholesterol reduction.
Post a Comment
Comment Moderation is ON ... I will NOT be routinely reviewing or publishing comments at this time..