Low HbA1c is as bad or worse than high HbA1c in non-diabetics
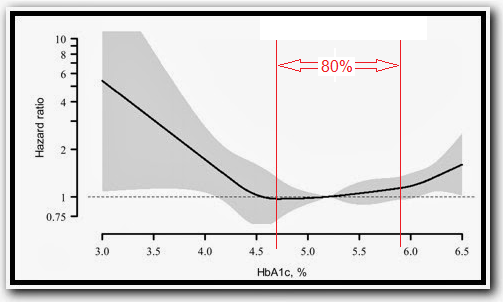
This study looked at roughly 14,000 NHANES III participants that were not diabetic. I think this is an important distinction because it looks at differences in normal range, "free", if you will, of what the frank hyperglycemia associated with metabolic dysfunction might do to mean and/or median values. Here is the hazard ratio plot:
To repeat from the caption -- HbA1c of 4.3% corresponds with the 2.5th percentile meaning only 2.5% of non-diabetics have levels this low (this percentage would be even lower for the entire population including diabetics). I would note that the 50th percentile (aka the median) is at 5.3%, but you go all the way up to the 90th percentile and reach a whopping 5.9%. Conversely you go all the way down to the 10th percentile at only 4.7%. It looks like the distribution is pretty uniform so I estimated the other major percentiles below (exact values shaded light gray):
The middle 80% of non-diabetics have a range of HbA1c from 4.7 to 5.9% ... a difference of a mere 1.2% ... the interquartile range is a mere 3/4ths of a percentage point!! The first reality about HbA1c, therefore, is that there isn't much difference in the normal range.
Excerpts:
... Participants with a low HbA1c (< 4.0%) had the highest levels of mean red blood cell volume, ferritin, and liver enzymes and the lowest levels of mean total cholesterol and diastolic blood pressure compared with their counterparts with HbA1c levels between 4.0% and 6.4%. An HbA1c < 4.0% versus 5.0% to 5.4% was associated with an increased risk of all-cause mortality (HR, 3.73; 95% CI, 1.45 to 9.63) after adjustment for age, race-ethnicity, and sex. This association was attenuated but remained statistically significant after further multivariable adjustment for lifestyle, cardiovascular factors, metabolic factors, red blood cell indices, iron storage indices, and liver function indices (HR, 2.90; 95% CI, 1.25 to 6.76).
Here's the mortality rate and hazard ratios (HR's)... The range of HbA1c values was 2.8% to 6.4%, and 97 participants had an HbA1c 4.0%. Participants with an HbA1c between 4.0% and 4.4% were the youngest; those with an HbA1c of 6.0 to 6.4% were the oldest (Table 1). A greater proportion of participants with HbA1c 5.0% were women. J-shaped or U-shaped associations were present for age, nonHispanic black race-ethnicity, less than a high school education, and annual household income $20 000. Mean cell volume, ferritin, transferrin saturation, and liver function measures were elevated in the HbA1c 4.0% group, whereas mean systolic blood pressure, diastolic blood pressure, total cholesterol, and median triglyceride levels were lowest among those with an HbA1c 4.0%. Also, the proportion of participants with a history of CVD disease was lowest among those with an HbA1c 4.0%, whereas the proportion of participants with hepatitis C was the highest in this group. ...
So HbA1c under 4 has HR twice that of the diabetics in this other study. Those with HbA1c between 4 and 4.5 had similar HR's to those with HbA1c's between 6.0 and 6.4.
If I had a very low HbA1c, I'd spend a bit more time looking at the different models, but note that the 97 with HbA1c < 4.0 represented only ~ 0.7% of people. This is rare. And it's associated with a significantly higher risk of all cause mortality compared to median HbA1c of 5.0-5.4%.
That low an HbA1c is an anomaly. Some seem to believe that the lower the better, right? Might brush off these HRs and mortality rates. Well, have a gander at the table below (this is from a study I discussed in considerable detail here). The numbers in parentheses in the population line represent the percent of the population in the study. Of particular note was that we don't see increased mortality (all cause or stroke) for the bottom 90% despite a significant range in postprandial glucose levels (note that the absolute values here do not translate well due to differences in analysis and glucose challenge). They expanded the top 10% across the right four columns and even then we're talking ~1.15, 1.3 and 1.6 for hazard ratios.

Let's not forget this study that found lowest all-cause mortality centered about a fasting glucose of 99 mg/dL. The plot at right might look familiar, those dots show the actual death rates. Below is the table of HR's for fasting glucose of 7.8 (140 mg/dL) or 7.0 (126 mg/dL) vs. 6.0 mmol (108 mg/dL) as reference, or 2 hour OGTT of 11.1 (200 mg/dL) vs. 7.7 (~140 mg/dL) as reference. Even compared to the higher unadjusted HR's, that HR for HbA1c below 4% is not looking so hot.
So what brought this up? Well, Fred Hahn asked a question on FB the other day, basically how a diabetic that resolves BG with a VLC diet can still be diabetic. This is somewhat of a topic (perhaps) for another day -- I've actually covered it quite a bit here. Basically I brought up pancreatic beta cell function and that basal hyperinsulinemia and the postprandial GSIS are not related (as I've discussed on here quite a bit. Some 800+ comments later, playing the "diabetes is a disease of glucose intolerance" card, along with the addict and Inuit cards, and Fred started another post:
...The one thing I found quite interesting in that thread was Evelyn suggesting that even though a low carb diet will help in the short term, the problem is finding a way to make the T2D able to handle carbohydrate. She said:
"It is a disease of relative insulin deficiency. Managing the hyperglycemia by lowering dietary carb simply manages the symptoms but does not fix the problem."
What problem is Evelyn talking about? The high carb eating T2D has *relative* insulin deficiency. Should the alcoholic try and find a way for his body to metabolize alcohol better so he can drink like every body else? Or should he stop drinking? Should the parents of a child with a severe peanut allergy try and find a way that their child can eat peanuts?
Why would a person need to find a way to be able to tolerate a large amount of carbohydrate in the diet? For what purpose?
Yeah, carbs, just like aflatoxin and alcohol ... but I digress. Dana Carpender entered the discussion: "The question is not are a low carb diet and exercise the only course of action that would benefit the patient, the question is do they offer the *most* benefit with the fewest risks." Now this gets frustrating because Dana is among the long term low carbers that have developed metabolic issues of late, and she does sport a list of health maladies that is not inconsequential. Though they can't all be blamed on her diet, there's simply no acknowledgement that her 75% on up fat diet that she aims might be a contributing factor. But her doctor was "startled and dazzled by my blood work." Not that there has ever been any proven benefit to an HDL over 100 or very low fasting triglycerides other than normal levels. She (and her doctor apparently) attribute her prior need for Metformin and Victoza and elevated FBG to gluconeogenesis from excess dietary protein .... which she has "fixed" by cutting that chocolate cake* protein down to 60-80 g/day (likely sufficient but at 20-30g carb per day that includes veggie carbs I wonder if lean mass will suffer over the long run and only she knows). (*a reference to Jimmy equating chocolate cake and steak in lectures)
But here was the boast that caught my eye:
And the impetus for me exhuming this study from my Mendeley files and publishing this up. I'm not sure I'd celebrate, but what do I know. Her low carb doctors tell her everything's stellar ... I'm sure they'll find something magical about ketones that renders this irrelevant.
And here is where these prospective studies and the FACT that there are no ... zero, zilch, none ever -- human populations consuming a diet remotely like hers or any of these other low carbers becomes important. We only have their reports to go by, and they aren't even encouraging. And yet they still promote this diet as healthy. And the doctors too. It's shameful, really.
As a dietary intervention LC has a great place. It's promoters harm that reputation by claiming the diet is superior or mandated for even a portion of the population. As a therapeutic measure it is generally used only in the short term, with supplementation I would add to prevent things like kidney stones that are otherwise extremely rare in the target population (e.g. epileptic children). That there are no known side effects other than constipation but let's compare to failed diabetes drugs and ignore that we have no long term data on LC diets (and the Inuit don't count (unless and until a new version centered on seal meat is implemented and promoted.)




Comments
I'm not even sure that LC diets truly have a "great place". If you look at some ultra low fat diets in which carbohydrate intake were not even controlled, as compared with standard ADA diet, glucose control was far better. I'm sure you know the studies better than I. How can a diet in which you are ingesting massive amounts of heme iron, saturated fat, cholesterol, methionine and likely other toxins have a 'great place'? Particularly when we don't know who will be harmed by it and who will be helped by it?
HbA1c, like the standard blood lipid panel, shows whether most people are responding normally to their common diet. When they respond abnormally, it may well indicate a disease. But when their diet is radically different from the norm, all bets are off.
It's not a question of whether buffoonery will happen but how many records of buffoonery can he break in one sentence?
My favorite was when his sister swooped in: Stop being so mean to my brother Freddy!! He's just trying to help people! LOLOL
Yes, HbA1c is, like cholesterol, pretty "meaningless" in the normal range. You can futz around with it and it will go a little lower or higher but in normal range it is a barometer of your metabolic health, not your diet.
RBC's run on glucose. We're not talking lowest decile here, we're talking lowest fractional percentile. But I guess low carbers don't need properly functioning red blood cells.
SO much rationalization it boggles the mind.
I'm not scared of fat or even saturated fat, but if you're getting more than half your calories from sat fat, I feel like you're maybe doing something wrong. Now bacon up that sausage, boy!
It's interesting that low HbA1c is a sign of disease, but how does this apply to low-carb? There was no low-carb arm in the study.
My HbAic is 5.4, Dan's was optimal on Atkins, even Dana's is only "<4" whatever that means.
Reading the discussion by the people who actually did this research, there is no mention of dietary carbohydrate, but discussion of multiple other factors - genetics, inflammation, infections. It is interesting that lower HbAIc is not always best, but you are jumping to conclusions that are not supported by the data.
http://homecooking.about.com/od/condimentrecipes/r/blsauce14.htm
http://homecooking.about.com/od/condimentrecipes/r/blsauce14.htm
Our systematic review and meta-analyses of worldwide reports suggested that low-carbohydrate diets were associated with a significantly higher risk of all-cause mortality in the long run. They also suggested that low-carbohydrate diets might not be protective or harmful in terms of CVD mortality and incidence. These
findings support the hypothesis that the short-term benefits of low-carbohydrate diets for weight loss are potentially irrelevant.
I too am fond of nuts, olives and avocados. There are no sources of dietary cholesterol in these, nor will you find heme iron, PAH's, HCA's, nitrites, growth hormones, estrogen, or antibiotics (though pesticides are possible). Also, it is not necessary to cause animal suffering in the form of massive factory-farms to get these to our plates at reasonable costs, but I will leave the ethical issues aside for now, since this is largely a health forum (I think).
Iron is actually reasonably absorbed from plant foods as non-heme iron if you are careful and put some thought into it -- avoid tannins at meal times, eat meals with vitamin C-rich foods, cook in iron cast pots and pans, eat iron-rich plantstuffs. It is impossible to get iron overload from plants since regulation of non-heme iron absorption so much better regulated than for heme iron. Heme iron is also a heavy oxidizer.
Whereas I used to think that a low carb high fat diet was optimal for health, I now think that a moderate-to-low carb plant based diet is optimal. But in this world, there are no 100 percents, and I look forward to being proven wrong.
I don't think there's any one diet that's optimal for everyone all the time. One individual might do better on a particular diet than another individual, and any given individual might do better with a different diet at different times. Right now I'm doing well eating lowish carb, but when my back gets a little better and I can start lifting heavy and higher volume again, I'll do better with more carbs.
I think people should be open to trying different diets to see what works for them, and not get too attached to any particular one, because things might change. I've seen a lot of people make themselves miserable by sticking with a plan that just wasn't working for them anymore.
IMO people should pay more attention to their moods and energy levels and freedom from pain and less to blood markers.
My ancestors lived in a place where unsaturated fats - other than fish - and starchy foods were not common items. Berries, honey, and hazelnuts would be the seasonal exceptions. Yet they were hardy and survived without knowing much about olive oil or avocadoes.
The vast majority of dietary interventions make absolutely trivial changes to diet (eg. swapping margarine for butter). The result is a trivial change to blood lipids.
Blood lipids are a DIETARY marker. They can be radically altered in a very short period (days to weeks) by MAJOR changes in diet. These changes are typically far faster than any major metabolic changes.
The blood lipid changes are predictable and reversible. eg:
- A high fat VLC diet significantly elevates HDL and lowers triglycerides.
- A very low fat vegan diet causes low TC.
Two of my biochemistry classmates performed a self-experiment involving a very high fibre/low fat/ 80%+unrefined carbohydrate diet back in the mid 80s. Both of them reduced their TOTAL CHOLESTEROL <2.5mm/L (180mg) within TWO WEEKS. The only noticeable health outcome was severe constipation (due to excess bran). The TC returned to normal (~5mmol/L) within 2-3 weeks of resuming a "normal" diet.
The makers of Flora Activ margarine actually admit that using their product reduces cholesterol levels but has NO measurable health benefits.
Surprise surprise, people who eat most deep fried food etc. have highest fat intake and highest mortality. But sugar and refined starch are still big part of their diet. These were all Western diets and none was prescribed. Paleo or LCHF were not popular enough among these populations at the time to influence the results
The fat in a donut is not its saving grace.
Have you tried oral liquid iron droppers? With those you can self-titrate just a drop or two at a time with each meal and thus limit your gut grief. One builds up one's tolerance very slowly. Unfortunately low carb does not love citrus, but vitamin C is available. Also there is randomized evidence that supplementing with lysine greatly improves iron absorption from non-heme iron. Do you cook tomato sauce in cast iron pots? That has also been shown to increase iron levels. There is a great deal of things you can do to increase your iron absorption from plants. Do you put blackstrap molasses in anything? only 3-4 g of CHO per teaspoon. Many anemics swear by it.
It is unfortunate that you need to eat red meat to get iron. Hope you have no family or personal history of colon cancer and are willing to do regular colonoscopy (starting at age 50, or earlier if relatives affected), supplemented by annual fecal occult blood testing.
A dietary intervention that takes one from abnormal extreme to normal or at least flirting with it is a positive change. When it moves you towards an abnormal extreme, perhaps it's time to re-evaluate.
If you're getting 50% or more of your calories from sat fat, then it's likely that your diet is almost entirely animal products, which means you're missing a lot of other good stuff. The point is not that animal products are bad. It's funny how when you argue in favor of variety and moderation, you get attacked from multiple sides.
Thank you for your concern, but I don't consider it unfortunate at all that I need to eat meat. Among other things, I get to support a local woman-owned business by buying it. I have no personal or family history of colon cancer, and the colonoscopy I had two months ago was completely clear, nary a polyp.
Humans thrive on a wide range of diets, the varied and the monotonous, the moderate and the extreme. Everyone's diet will seem extreme to someone else. There's no need to tut tut over it unless the diet is obviously producing disease (there are many many other causes of disease). The SAD, vegan diets, the nutritional deficiency diets of the very poor, and so on are worth tut tutting over.
Diets on which individuals thrive are not. In many parts of the world humans evolved on necessarily limited diets, but as long as they had access to animal foods this didn't matter, because animals will collect every nutrient an animal needs or die trying.
When you argue in favour of one concept, even variety and moderation, you are arguing against all the others, so of course there is dispute. If I wanted my views to be accepted unchallenged I would post my comments somewhere else.
Yeah, that's actually not my point at all. I probably should have phrased it more clearly rather than trying to be cute about it. What I mean is not that my ideas are being attacked, but that straw men are. Apparently I'm simultaneously eating a diet packed with massive amounts of sat fat and arguing against same, depending on who you ask.
Butter does contain vitamin A, for example, but much less than a carrot. The carrot is very low in calories, compared to the butter. Toss the shredded carrot with a bit of olive oil - in fact, just make it part of a salad of fresh vegetables with a salad dressing, and you get all the vitamin A for a lot fewer calories. The carrot will also have lutein and Zeaxanthin. A small red tomato is going to be a similar bargain.
Fermentation of fiber in the gut is going to produce butyrate.
I love butter. I mix it half-and-half with canola oil. But I love my veggies more!
Fats can be very cytotoxic. You are aware that unlike carbs that do burn efficiently and fully, there are fatty "byproducts" such as ceramides and diacylglycerols that are not so mitochondria friendly.
That's certainly the first time I've ever heard that a vegan diet is worth tut-tutting over. Why? Because it's been proven to regress coronary disease (a la Ornish and Esselstyn), exerts a tiny ecological footprint compared to pasturing meat, and doesn't cause animals to suffer needlessly? The only reason you say vegan diets are worth tut-tutting over is because you have no idea what a vegan diet actually is (beyond the 'headlines'). It can actually be incredibly varied with the only vitamin missing being B12 (which can easily be supplemented or consumed in the form of fortified foods). Yes, I used to think the same way you do, that an omnivorous diet is best. But I am getting the best of all possible worlds on a vegan diet - limited saturated fat intake, no dietary cholesterol, no highly oxidative heme iron, no "natural" TFAs, no PAH/HCA's from meat searing, no antibiotics, growth hormones, estrogen, much less environmental impact (and I do support local farms), and no animal suffering to justify or ignore. On the other hand you get many things that animal-based diets typically lack - phytochemicals, flavins/flavanoids, antioxidants, fibre, phylloquinone, folic acid, polyphenols galore, etc. At least the research is on my side.
(I realize I am in a tiny minority - only 2% of the population identifies as vegetarian or vegan, but these numbers are skyrocketing. )
A point that can't be stressed often enough. Stunted growth is common for epileptic kids ... I really worry what these menopausal women and even the younger ones that are restricting protein now too are doing to their bones.
This may not be enough to cause noticeable symptoms but that doesn't mean everything's hunkey dorey. If she were my friend or I thought she'd listen to me, I'd point these things out to her.
http://www.ncbi.nlm.nih.gov/pubmed/10050267
"Thus the hypothesis that colonic iron, bile acids, or total fatty acids can promote colon tumors is not supported by this study. The results suggest that, in rats, beef does not promote the growth of ACF and chicken does not protect against colon carcinogenesis. A bacon-based diet appears to protect against carcinogenesis, perhaps because bacon contains 5% NaCl and increased the rats' water intake."
there are also animal studies in which inulin (prebiotic plant fibre) promotes cancer growth. Burnt/charred meat, you can maybe make a case, but If I had to choose dietary risk factors for colon cancer to avoid they would be alcohol, sugar, and flour.
http://cebp.aacrjournals.org/content/6/9/677.abstract
Those at greatest risk from a high dietary GI were those who were sedentary (for men, relative to those who were most active and had a low-GI diet: OR, 3.46; 95% CI, 1.78-6.70; for women: OR, 2.00; 95% CI, 0.98-4.07). We also observed that people who had a high sucrose: dietary fiber ration and who also were sedentary and had a large body mass index were at increased risk (OR, 4.58; 95% CI, 2.33-8.98) relative to those who had a low sucrose:dietary fiber ratio, were active, and had low body mass indices. These findings support previous reports that dietary sugars, especially diet high in simple carbohydrates relative to complex carbohydrates, increase risk of colon cancer, possibly through their impact on plasma glucose levels.
OR 4.58 is a whopping correlation. Any correlation with meat is either much smaller, or is simply not seen at all, as here: http://www.ncbi.nlm.nih.gov/pubmed/8123778
"Fatty acids are ligands for PPARs, so it is possible that the large amounts of fatty acids liberated from the adipose tissue can stimulate their own metabolism by activating PPARa" - this mainly happens in fasting or carbohydrate restricted states, but DHA probably retains some efficacy in presence of glucose.
http://tiny.cc/PPAR-alpha
As for, was it the diet or the other x factors? Maybe it was a synergy between all those elements. Maybe. . . Just, maybe, a whole foods 10% fat diet can be quite healthy. And maybe, just maybe, a grounded and supplemented vegan diet--knowing that it's built on compromises--can also be healthy and beneficial.
Hh. Adorable stuff. . . One person makes a blanket statement about vegan diets (tut tut deficient, bad, SAD conflate-worthy) and then another one makes a blanket statement about omnivorous diets (devoid of phytochemicals, etc.).
LOL!
http://jco.ascopubs.org/content/31/22/2763.long
Post a Comment
Comment Moderation is ON ... I will NOT be routinely reviewing or publishing comments at this time..