My Gut Feeling on Microflobesity Was Right
This post brought to you by Duck Dodgers' arrogance. If there ever were an example of what is wrong with science in the Incestral Health Community, it is the phenomenon that is "Duck Dodgers" and his comments here. A seemingly non-controversial post -- on how the US Dietary Guidelines were never any radical departure from the way humans around the globe have eaten for thousands of years -- went viral, at least in part because of Duck's return. What rubs me personally the wrong way about this person (or persons, though I've been told it is only one person who posts with that ID in comments here so I operate on that assumption) is his response to any challenge to "How Food Enrichment Made Us Fat, Diabetic, and Chronically Diseased" otherwise known as the "Iron Food Enrichment Hypothesis". Despite doubling down on the whole fortification thing at the off-the-grid web rental only around a month ago, this guy comes on here and plays word games regarding whether it is even a theory or hypothesis. Duck behaves as if I somehow owe it to him and the internet to take his unscientific self seriously, and if I don't take him and his ideas seriously it can only be that I find them inconvenient to my comfortable mindset.
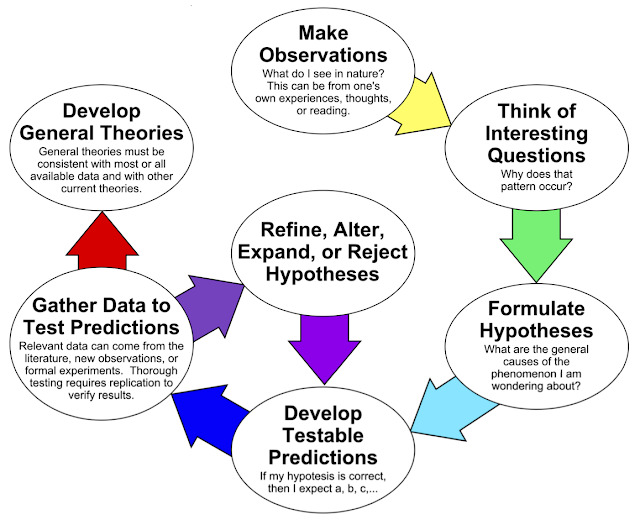
I have wasted enough time on this whole nonsense, if anyone wants at it they know full well where they can go to discuss it. I don't dabble in non-scientific mumbo jumbo and I laid out some general thoughts on this in this post: Science ... .
I'm going to try to summarize the gist of the conversation without rehashing the whole thing. Folks should know that I probably read at least half of the comments on this blog in email. This is what I remember. And this was the first sentence of Duck's first comment on the post:
I think this was a good post, but it didn't swing for the fences.
He later edited that out (see updated Comment Policy), and left the enrichment part. There is actually some relevance to enrichment and the Dietary Guidelines, but unfortunately Duck was unable to focus on that. This devolved into such lovelies as "And frankly, would it really kill you to have an open mind and consider that Jane maybe found something that's worth a closer look—as a friend would do?" This is after numerous comments in response to Jane, Duck and others on both this thread and the prior one that was hijacked demonstrating that I HAVE given this a closer look. What I found were innumerable problems with the hypothesis, theory, puzzle, whatever they want to call it that ultimately settled on mineral imbalance. Then I showed data from studies where the obesity inducing diet had the preferable mineral profile to the standard rodent chow.
I also looked into the hypothalamic obesity. This has been far more than just a quick glance, and I want to co-publish two posts so there may be more of a delay in doing so. I'll say this much here and now: there's nothing in the literature as yet supporting dietary iron excess (or imbalance) → iron overload in hypothalamus → damage of hypothalamus → the hyperphagia of hypothalamic lesion → obesity. There is ample evidence that tissue iron overload is a symptom, not a cause, though I doubt I devote much time to that unless it comes up again in another context. But those posts won't be about iron, they will be about whether the mechanisms of hypothalamic obesity are relevant to "ordinary obesity" -- is hypothalamic damage the initiating factor? In the interests of not hijacking that discussion prematurely, I'll save my thoughts.
So here was one of my final comments on that post:
click to view larger ... I am not going to waste my time further here. I've looked back at enough animal studies that were discussed previously here testing some other hypothesis and pointed out several, now, where the mineral imbalance notion doesn't fit. You cherry pick what you can make fit, you ignore the rest.I hope you'll read my post on hypothalamic damage when it comes out. ...
I'm hopeful the whole point of the article(s) won't be to just sweep this under the rug in some quick dismissal so that you can go about sticking to comfortable theories.
Allow me to paraphrase from my Science post, not every idea deserves even the time of day, let alone any sort of thorough looking into. Coming from Duck after he just "quickly dismissed" several facts-in-evidence directly countering his "comfortable theory", was just a bit much for me. So Duck had taken me up on my offer to read some of my blog. What did he do? Look into what I blog a lot about? Perhaps learn a thing or two about science? No. He decided to see what I have written about another pet interest of his blog host, the gut biome.
I took it upon myself to read your take of the microbiome—a burgeoning area of interest in the world of obesity and metabolic issues.
Actually, it's more of a burgeoning area of interest in the *industry*. As in, it's an area of burgeoning profiteering for the snake oil salesmen. No wonder it's so popular in the IHC.
OK so I later had to ask what these were, and as it turns out, Duck has found his way back almost 5 years of blogging to the following:For the few times you've ever mentioned the microbiome on this blog, it felt like you basically took it upon yourself to sweep the entire microbiome under the rug with a two-part post.
- Of Mice, Men & Microflora I: The microflora transplant study
- Of Mice, Men & Microflora II: Microflora & Energy Balance
Dismissing new perspectives seems to be the name of the game here. I thought that seemed rather hasty and I personally think it shows a lack of interest in challenging your own ideas. (I wouldn't have engaged in a conversation here if I wasn't interested in getting outside of my own comfort zone).
Ahh yes, Duck is such an open-minded chap, while I'm sitting here in my comfort zone deleting the majority of comments and blocking those who disagree with me and challenge my supremely narrow beliefs because I cannot deal with it. [ /snarkism ]
Don't look now, but five years ago I wrote not one but two blog posts on the topic. How is that "rather hasty"?
And?There is so little we still know about the microbiome, but it's importance has already shown to be quite bigger than anyone ever previously imagined. And, whattaya know, our microflora influence the way we absorb micronutrients, like iron.
On the other hand, many major scientific discoveries are often ridiculed and dismissed when they are first examined by the established science. You certainly wouldn't be the first to dismiss something important—happens all the time.
Oh yeah, the whole "first they ridiculed ..." nonsense. Too bad studies have shown that 999,999 out of 1,000,000 times, that's not how good science happens. I'll leave you to follow faddists like the host of your content Duck, and I'll stick with what the emerging evidence tells us, as it becomes available. Mmmkay? Let's look at those posts briefly.
 This post focused on the observations of weight gain when one transplants bacteria from a normal or obese mouse into a germ-free mouse. As hindgut fermenters, rodents rely on energy extraction from food done by the bacteria in their functioning cecums. If a normal mouse and a germ-free mouse consume the same amount of a standard rodent chow, the normal mouse will gain more weight. This is simple physiology and thermodynamics. The normal mouse has access to and absorbs more calories due to their microflora breaking down otherwise indigestible matter in their food. Thus for the hindgut fermenter, "energy harvest" by the microbiome is a significant contributor to their nutrition.
This post focused on the observations of weight gain when one transplants bacteria from a normal or obese mouse into a germ-free mouse. As hindgut fermenters, rodents rely on energy extraction from food done by the bacteria in their functioning cecums. If a normal mouse and a germ-free mouse consume the same amount of a standard rodent chow, the normal mouse will gain more weight. This is simple physiology and thermodynamics. The normal mouse has access to and absorbs more calories due to their microflora breaking down otherwise indigestible matter in their food. Thus for the hindgut fermenter, "energy harvest" by the microbiome is a significant contributor to their nutrition.
There was absolutely nothing amazing, groundbreaking or magic about that in 2010. In that post I linked to An obesity-associated gut microbiome with increased capacity for energy harvest, which was a 2006 study taking things a step further. They did the transplants into the same germ-free mice from either ob/ob mice or lean mice. The ob/ob-microflora recipients gained more weight/fat than those receiving microflora from the lean mice. Aha!
Not so fast ...
This post looked at the energy balance explanation for what was observed. It's not like it wasn't telegraphed in the title: "energy harvest". You ready?
 |
| "Our results indicate that the obese microbiome has an increased capacity to harvest energy from the diet." |
So you add bacteria capable of extracting more energy into a germ-free mouse and it gains more weight. Call me dismissive all you want as you dismiss the straightforward explanation of the researchers! It is consistent with CICO with zero need for wild speculation. Which leads me to my usual question ...
How Does This Apply to Humans?
Still in that second blog post, I asked this very question. In general terms, given the numbers of fecal transplants that had been done to date for C.dificiles infections, surely there must have been more than a few of these transplants that involved lean donors and obese recipients. Nobody reported miraculous weight loss following a FMT??
How about a study doing just that? I linked to this report that discussed one in humans: Transfer Intestinal Microbiota From Lean Donors Increases Insulin Sensitivity in Individuals With Metabolic Syndrome. (I don't see that I linked to this directly it in the 2010 posts, I have seen it before now, but have no idea when it was originally saved to a hard drive). This was touted quite a bit about the IHC at the time, but dismissive me was apparently the only person inquisitive enough to wonder exactly what the results were. The researchers introduced fecal matter obtained from lean men into obese men, and compared this with a control group receiving a "transplant" of their own fecal matter. The main findings were:
- Virtually no changes after six weeks in either group for pretty much everything.

- To stress: NO CHANGE IN WEIGHT (or anything else for that matter)
- No changes in intake, REE, etc.
- Changes in some strains of bacteria, increasing butyrate producing bacteria in those receiving the lean FMT.
- Improvement in peripheral insulin sensitivity as measured by hyperinsulinemic-euglycemic clamp.
I looked back from time to time for a follow-up to see if this inconsequential finding (undetected by any of the usual means -- see table above) persisted past 6 weeks. Never could find anything. Some may say 6 weeks is not long enough to see weight loss, but if that were the case, surely when these subjects lost all this weight we'd have heard about that? No.
See, this was an early sign of direction of cause and effect in the association. It seemingly went ignored by those captivated by the notion that gut bacteria could be the cause of our obesity epidemic. It certainly seemed to be a positive to have something about insulin resistance in the mix! The gut flora could simply be one more means by which carbohydrates wield their destructive obesogenic powers. I didn't note this a the time, but this was actually early evidence outside of Taubes' own references and existing clinical trials manipulating calories and macronutrients. This study showed that changes peripheral insulin resistance, measured as glucose disposal into peripheral tissues -- aka glucose uptake into muscle cells, had no impact on weight or any other metabolic parameters of dysregulated glucose metabolism. Put another way, if the "clogged sink" backup model of insulin resistance were valid, then according to TWICHOO improving disposal into muscle, alleviating hyperglycemia and lowering the amount of insulin needed to be secreted to clear glucose should result in weight loss.
Before moving on, Duck must have missed where the same day as Mice II, I posted a short post of links, one of which was to the "state of the knowledge" circa 2010. You will note that the "obese microbiome" is in and of itself a controversial issue. The same patterns aren't always seen. Despite discussing numerous other avenues vis a vis insulin sensitivity and overall metabolism, etc., the paper concludes as follows:
Before moving on, Duck must have missed where the same day as Mice II, I posted a short post of links, one of which was to the "state of the knowledge" circa 2010. You will note that the "obese microbiome" is in and of itself a controversial issue. The same patterns aren't always seen. Despite discussing numerous other avenues vis a vis insulin sensitivity and overall metabolism, etc., the paper concludes as follows:
Intestinal microbiota may play a pivotal role in converting nutrients into energy. Variations in the composition of microbiota are found in obese humans and mice. Increased energy yield from diet in obese mice and humans could be a contributing factor to obesity, although the pathophysiological processes driving this bidirectional relationship have not been fully elucidated.
The scientists actually studying obesity are not so easily swayed by faddish ideas. They know that whatever is "there" must have a plausible mechanism. Ultimately, energy balance must be honored in the construction of that mechanism.
To that end, somewhere on this blog I've linked to the academic source of this estimate, but I cannot find it at the moment, and I'm short on time. Humans, lacking a functioning cecum, and not being ruminant animals, have a very limited capability for extracting energy from fiber via the gut microflora. Your very plant-heavy eater may feasibly get as much as 5% of their energy from bacterial "fermentation". But working with that figure is misleading in my opinion. Let's look at our modern diet, with its low fiber content of around 15 grams (recs are 25g for women and 38g for men , in many studies you will see reports in the 20s, even the Lindeberg paleo!). If you had very effective energy harvesting bacteria, that's at most 60 calories. But for humans, we're averaging about half that (again, at most because insoluble fiber is still largely indigestible). The caloric differential between lean and obese is likely to be only a fraction of this maximum.
What about simple carbohydrates, methanogens, and whatnot? If your gut flora are feeding on undigested sugars and starches -- that would otherwise be digestible with your human physiology and digested by you -- then these are "calorie sinks" not "energy extractors". Whatever comes "out" of the bacterium will have less caloric energy than what went "in". (This is true in all cases, it's just that when the bacteria converts indigestible substances into usable calories, it is a net positive for the host, e.g. you or me.) Let's throw this into the mix: Obesity is associated with a higher methanogenic (methane-producing) bacteria. Don't look now, but that's more calories out undigested/unabsorbed and thus unavailable to become body fat.
Is there anyone still reading this who is wondering why I don't devote more time and blog posts to this line of investigation?
While many in the IHC are busy sending their crap off in kits to various testing facilities, making sure to use affiliate links of their favorite guru who literally doesn't know shit, I'll refrain from encouraging same. If you think you have an intestinal bacterial issue, please get it diagnosed and treated by someone trained and experienced in doing same. That is, after all, how these fecal transplants even came about.
But before I go, I'ma gonna gloat....
Nah nah na na nah naaaahhhhh ... Vindication!!!
Changes seen in gut bacteria content and distribution with obesity: causation or association? (request full text)
In both humans and animals there are characteristic changes in the gut microbiota associated with obesity. In animals but not in humans altering the microbiota can result in weight loss and weight gain which does not occur in humans.
This suggests that in humans the changes in gut microbiota are an association with rather than the cause of obesity.
What follows is a significant excerpt of the last paragraph of the discussion and the summary conclusions, beginning with the last paragraph I have taken the liberty to format for emphasis:
It is highly unlikely that fecal transplantation would be used in humans to treat a chronic non-life-threatening condition such as obesity. The one and only significant fecal transplant study which addressed only insulin resistance was first presented at the European Association for the Study of Diabetes meeting in Stockholm in 2010 and 2 years later was published in Gastroenterology.[31]
Ref. 31: Transfer of intestinal microbiota from lean donors increases insulin sensitivity in individuals with metabolic syndrome. (does not appear much different from thesis at first glance)
The study involved 18 insulin-resistant nondiabetic men who without a change in diet or activity and who after bowel cleansing received by nasogastric tube either an autologous fecal transplant or a fecal transplant from a lean male donor. This study showed a decrease in the median rate of glucose disappearance in those who received a fecal transplant from a lean donor compared with those who received an autologous fecal transplant (26.2–45.3 dmol/kg·min) without significant weight loss.The improvement in insulin sensitivity was only temporary since when retested 12 weeks later the rate of glucose disposal had returned to the baseline level which was similar to the glucose disposal rate in the autologous fecal transplant group.[31]
Yeah, that's the 2010 study everyone was all so excited about in the IHC. It's going to be all about the gut biome soon. Mark Sisson's words (double entendre intended). Paleo will own it by the power of Zonulin! (three guesses who I'm referring to there ...). One study in humans. The results of which were so encouraging to actual scientists that more are in the works? Well, it's 2015. A search on clinicaltrials.gov nets 40 hits. Unless I missed some, 38 deal with gastroenterological issues such as ulcerative colitis, Crohns, and C. dificiles. None deal with obesity. Two deal with metabolic syndrome:
- Transplantation of Microbes for Treatment of Metabolic Syndrome & NAFLD (FMT). Just submitted July 2015! Looks to be a longer term (6 months) repeat of the 2010 study, 9 autologous, 12 FMT from lean. They are not yet recruiting, starting in January though. Estimated completion data collection Sept. 2017, study Dec. 2017. If you don't see another blog post on this until 2018 if I'm still blogging, you'll know why ;-) If the effect didn't last for 12 weeks in the prior study ....
- Fecal Microbiota Transplantation on Type 2 Diabetes Mellitus. This one was initiated in 2012 and today's status is "this study is enrolling participants by invitation only". It was scheduled to end earlier this year. Not holding breath. It appears to be an uncontrolled study utilizing transplant via endoscopy.
And now ... (again formatted slightly for emphasis)
Summary and conclusions
There is clearly in both animals and humans changes in the gut microbiota that are associated with obesity. In animals the transfer of these obese microbiota to germ-free animals causes the development of obesity. However, in humans the available evidence would suggest that the differences in the gut microbiota that are associated with obesity probably result from the utilization of a high-calorie, high-fat and high-carbohydrate Western diet.
Therefore, it is most likely that the typical obesity microbiota is an association with dietary intake rather than being a cause of obesity.
In both humans and animals environmental changes such as changes in diet, utilization of artificial sweeteners, decreased exercise and disrupted diurnal rhythm will quickly convert the microbiota to that of an obese pattern. In addition, dietary changes that occur following a gastric bypass most likely account for the changes in the microbiota from an obese to a lean gut microbiota pattern that occur with this surgery. However, the possibility that because of gastric bypass surgery, FXR is downregulated resulting in decreased bile acid production which allows for regrowth of bacteria which facilitate weight loss should also be considered.
If it is believed that obesity occurs as a result of an obese microbiota pattern rather than the obese microbiota being a marker for the obese state, large studies utilizing either probiotics or prebiotics should be performed since for ethical and practical reasons a study of fecal transplantation would be difficult to perform in humans who are neither acutely ill nor have a “life-threatening” illness. However, now that a fecal capsule which can be swallowed is available fecal transplant could in the future become more acceptable and could be tested in the obese human.
Currently, the outcomes of prebiotic and probiotic utilization in the treatment of human obesity are less than convincing and certainly do not match the studies performed in animals.
A large, blinded, randomized study could and should be performed utilizing either prebiotics or probiotics. If any of these studies showed positive results utilization of prebiotics or probiotics or even fecal transplantation or bacterial components of a healthy stool could be utilized to avoid or reduce the number of bariatric surgeries being performed which would result in substantial savings to the health-care system and decreased morbidity and mortality.
My Concluding Thoughts
The scientists have plodded along with their method for the most part. They made some observations of associations. Despite early indications that the obese microbiome was not consistent in humans, they continued. Experiments were conducted on germ-free mice and the results were consistent with a role for gut microflora in energy balance these rodents.
But in the one study in humans, it failed to translate. The main reason why is likely in my first post on the topic:
Rodents use bacteria to extract SIGNIFICANT energy from their food, humans do not.
There are other things that factor into the nuances of energy homeostasis in rodents that are not in play or differ substantially in humans. These are:
- Rodents have substantial metabolically active brown fat.
- Rodents expend a much higher proportion of total energy on maintaining body temperature.
- Rodents can dial this down or ramp it up to maintain homeostasis to a greater extent.
- Human brains require a much higher proportion of total energy expenditure.
- Human white fat depots differ in size, location and proportion from rodents and there is great variability across the species on a gender, age, race and individual basis.
- Did I mention humans don't have a lot of brown fat?
- ... etc. etc. etc.
Here's one references from one of these papers you who are still interested in learning about making germ-free mice fatter or leaner:
Mechanisms underlying the resistance to diet-induced obesity in germ-free mice (2014)
Together, these findings support the notion that the gut microbiota can influence both sides of the energy balance equation, and underscore the importance of considering our metabolome in a supraorganismal context.
I disagree. Your mileage may vary. My intuition appears to have been on target in 2010. My mind IS open to change when presented with reputable evidence to reopen the case. Have I missed anything?? Your comments are welcome. Link away to stuff about the gut biome. Keep it on topic or even regale me with your personal experiences and microbiome results. I think it's obvious what I have left off the list here that I am not interested in hearing more about at the moment.


Comments
Post a Comment
Comment Moderation is ON ... I will NOT be routinely reviewing or publishing comments at this time..