Blood Sugar 140: Context is Everything I - Diabetic vs. Non
In Blood Sugar 140: Where did the 140 mg/dL threshold come from?, I laid some groundwork as to the source of the concern over postprandial blood glucose levels over 140. Before moving on, I thought I'd share an additional example of the 140 mg/dL threshold being evoked. Here is a thread on Dr. Dansinger's WebMD diabetes forums: glycation damage.
I ask this question because the consensus is that blood sugars over 140 cause the sugar to stick to vessels and organs. Dr. Gabe Mirkin writes of this on his web site. Others like John McDougall do not seem to worry about sugars over 140.
I can understand that you don't want fasting sugars over 140 but apparently even postprandials over 140 cause damage. I am wondering how long it would take for damage to be recognizable if post prandials are above 140. And does it matter how long they remain over 140 after eating?
... A corollary to this would be the question --if you can keep your blood sugars at all times below 140 does this guarantee that you will not get complications--whether by means of diet, exercise, meds or any combination of treatments?
... I never worried about this until reading on this group that sugars shouldn't go above 140.
Now I looked for the Dr. Mirkin reference and found a lot of info, but not specifically referring to postprandial levels other than that the current guidelines use a cut-off of 140 mg/dL at the 2 hour mark of an OGTT for a diagnosis of impaired glucose tolerance, IGT. Others in that discussion pointed out that it wasn't all pp levels, but the 2 hr level for an OGTT. Jenny Ruhl's site is also brought up. (As an aside, one Mirkin hit was a blog curation site that directed me to this post by Wheat Belly, pre-book bonanza. Seems back in 2008, a bowl of Cheerios only surged BG to 140, in 2011, a bowl of oatmeal would typically cause a surge to around 180!).
I want to make a few things clear before moving on with this series. This is not an anti-Jenny, anti-Paul or anything of the sort. It is intended to dispel some of what I see as anywhere between unnecessary concern to downright paranoia over the "toxic" effects of glucose cultivated in the low carb community. In some cases I see this taken out of context, but it is fair to say that Jenny's writing (on the website anyway, I haven't read her book) can tend towards unwarranted hyperbole at times (e.g. calling the crash diet dangerous and idiotic), but many take her advice to diabetics out of context as well, to apply to their non-diabetic existences. Paul seems to go out of his way not to offend or to take every possible objection to including starch in his diet into consideration, and I think this is "to a fault" at times. It is very easy to get sucked into this glucose is toxic, we're all diabetic mindset, especially if one gets under the influence of someone like Wheat Belly who believes one's blood sugar should be at pre-prandial levels within an hour of eating any meal. I was pretty convinced in 2009 that I must be IR at least and boy was I shocked to discover I had dead nuts normal glycemic control eating high or low carb. If anything I think I have some minor insufficiency for gluconeogenesis -- AM hypos, especially exercising in the morning when VLC, were likely my issue several years back.
I tend to agree with those who view the targets given to diabetics as being too permissive, and can understand the desire of diabetics to seek out a safe glucose level -- the "corollary" question in that WebMD exchange. In that light, the 140 pp target is a far preferable goal compared with than the current recommendations:
This is where I think Gary Taubes has been most damaging to the discussion in demonizing a hormone required for life! Insulin does more than just act on fat cells, it prevents catabolism of and promotes growth of lean tissues like muscle and bone. Many of the reduced diabetic complications seen in patients with better glycemic control may well be due to the fact that better glycemic control often involves proper insulin dosing. Advances in insulin therapies -- injection methods, pumps, long-acting, etc.etc. -- have dramatically improved the ability of diabetics to not only meet ADA targets, but obtain truly "normal" glycemia. I will address this point in a later post in this series, but I can think of nothing more harmful to health than the insulin phobia rampant in the LC community. While the frank type 2 diabetic is baseline hyperinsulinemic, they don't produce the appropriate acute insulin response. Given the health issues accompanying improper insulin/signaling, it seems a no-brainer that establishing as normal a level of both insulin and glucose as possible.
So anyway, after my exchange with Karen (a diabetic) on the first post, I split this Context post in two in order to address the relevance of the 140 mg/dL level for diabetics vs. non-diabetics, and in the next part I'll address the context of that level in terms of the OGTT to which it applies. Back to topic at hand.
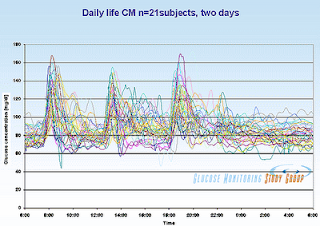 Whenever talking normal glucose levels, I'm always reminded of Ned Koch's post from which the graphic at right comes. These are glucose levels in non-diabetics taken over the course of two normal days. Now, granted not all seemed to even exceed the 140 threshold, but many. If it were true that nerve damage occurs at glucose levels over 140, certainly cumulatively over time, we'd be seeing neuropathy more in the general population.
Whenever talking normal glucose levels, I'm always reminded of Ned Koch's post from which the graphic at right comes. These are glucose levels in non-diabetics taken over the course of two normal days. Now, granted not all seemed to even exceed the 140 threshold, but many. If it were true that nerve damage occurs at glucose levels over 140, certainly cumulatively over time, we'd be seeing neuropathy more in the general population.
This is a very important point. Normal individuals eating a "normal" diet will regularly exceed 140 mg/dL, though not necessarily by much, to no apparent detriment. Neuropathy would simply be far more common in occur in younger populations if BG's over 140 damaged nerves to any significant level.
In a diabetic, however, not only do postprandial glucose levels climb higher, they tend to stay elevated for longer periods of time, thus if the hyperglycemia is toxic per se, the exposure is greater. The glucose levels also may never fall below, say, 100 or even far higher depending on the degree of glycemic control. Therefore it is not surprising that IGT or diabetes was diagnosed by OGTT in 2/3rds of subjects presenting with neuropathy in this study. I shall discuss the implications of that finding in a separate post as well.
I want to make a few things clear before moving on with this series. This is not an anti-Jenny, anti-Paul or anything of the sort. It is intended to dispel some of what I see as anywhere between unnecessary concern to downright paranoia over the "toxic" effects of glucose cultivated in the low carb community. In some cases I see this taken out of context, but it is fair to say that Jenny's writing (on the website anyway, I haven't read her book) can tend towards unwarranted hyperbole at times (e.g. calling the crash diet dangerous and idiotic), but many take her advice to diabetics out of context as well, to apply to their non-diabetic existences. Paul seems to go out of his way not to offend or to take every possible objection to including starch in his diet into consideration, and I think this is "to a fault" at times. It is very easy to get sucked into this glucose is toxic, we're all diabetic mindset, especially if one gets under the influence of someone like Wheat Belly who believes one's blood sugar should be at pre-prandial levels within an hour of eating any meal. I was pretty convinced in 2009 that I must be IR at least and boy was I shocked to discover I had dead nuts normal glycemic control eating high or low carb. If anything I think I have some minor insufficiency for gluconeogenesis -- AM hypos, especially exercising in the morning when VLC, were likely my issue several years back.
I tend to agree with those who view the targets given to diabetics as being too permissive, and can understand the desire of diabetics to seek out a safe glucose level -- the "corollary" question in that WebMD exchange. In that light, the 140 pp target is a far preferable goal compared with than the current recommendations:
Less than 180 but high enough that hypoglycemia won't result from any "onboard" insulin if testing at only 1-2 hours.The recommendations are skewed towards insulin-dependent diabetics for whom hypoglycemia is a very real possibility and more immediately life-threatening than for non-insulin using type 2's. What really bothers me, however, is the derision for using insulin at all in the community. If someone is insulin deficient -- and a T2 can be both hyperinsulinemic at baseline and GSIS-impaired -- low carbers should not be so hostile towards those who use it. By that I mean since practically day one of finding this online community I was hearing diabetics derided for not wanting to see the light and insisting on eating carbs and just covering it with insulin. It's like "I care about my health", "my stupid fill-in-the-blank just wants to eat crap and take medications" and all my doctor wants to do force carbs on me and hand me prescriptions.
This is where I think Gary Taubes has been most damaging to the discussion in demonizing a hormone required for life! Insulin does more than just act on fat cells, it prevents catabolism of and promotes growth of lean tissues like muscle and bone. Many of the reduced diabetic complications seen in patients with better glycemic control may well be due to the fact that better glycemic control often involves proper insulin dosing. Advances in insulin therapies -- injection methods, pumps, long-acting, etc.etc. -- have dramatically improved the ability of diabetics to not only meet ADA targets, but obtain truly "normal" glycemia. I will address this point in a later post in this series, but I can think of nothing more harmful to health than the insulin phobia rampant in the LC community. While the frank type 2 diabetic is baseline hyperinsulinemic, they don't produce the appropriate acute insulin response. Given the health issues accompanying improper insulin/signaling, it seems a no-brainer that establishing as normal a level of both insulin and glucose as possible.
So anyway, after my exchange with Karen (a diabetic) on the first post, I split this Context post in two in order to address the relevance of the 140 mg/dL level for diabetics vs. non-diabetics, and in the next part I'll address the context of that level in terms of the OGTT to which it applies. Back to topic at hand.
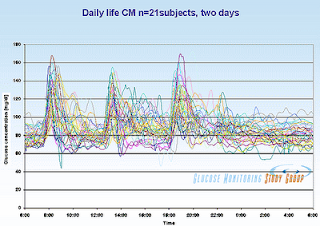 Whenever talking normal glucose levels, I'm always reminded of Ned Koch's post from which the graphic at right comes. These are glucose levels in non-diabetics taken over the course of two normal days. Now, granted not all seemed to even exceed the 140 threshold, but many. If it were true that nerve damage occurs at glucose levels over 140, certainly cumulatively over time, we'd be seeing neuropathy more in the general population.
Whenever talking normal glucose levels, I'm always reminded of Ned Koch's post from which the graphic at right comes. These are glucose levels in non-diabetics taken over the course of two normal days. Now, granted not all seemed to even exceed the 140 threshold, but many. If it were true that nerve damage occurs at glucose levels over 140, certainly cumulatively over time, we'd be seeing neuropathy more in the general population.This is a very important point. Normal individuals eating a "normal" diet will regularly exceed 140 mg/dL, though not necessarily by much, to no apparent detriment. Neuropathy would simply be far more common in occur in younger populations if BG's over 140 damaged nerves to any significant level.
In a diabetic, however, not only do postprandial glucose levels climb higher, they tend to stay elevated for longer periods of time, thus if the hyperglycemia is toxic per se, the exposure is greater. The glucose levels also may never fall below, say, 100 or even far higher depending on the degree of glycemic control. Therefore it is not surprising that IGT or diabetes was diagnosed by OGTT in 2/3rds of subjects presenting with neuropathy in this study. I shall discuss the implications of that finding in a separate post as well.
In someone with impaired insulin secretion (T1 = none/insignificant, T1.5 = insufficient, T2 = varying depending) if blood glucose goes over 140, it likely climbs considerably over that and takes longer to clear (and/or is added to by inappropriate endogenous glucose production). The more carbs ingested the higher the glucose spike in somewhat proportional fashion. This is because insulin is not secreted properly and the glucose will be cleared by non-insulin dependent mechanisms. A person with normal insulin secretion will almost never get a glucose spike over around 180 because their glucose stimulated insulin secretion (GSIS) is proportional to the glucose ingested. So a diabetic consumes 50g carb or 100g carb and their BG level climbs quite a lot higher after the 100g load, but a non-diabetic consumes 50g or 100g or 200g, and their BG level may climb 10 or 20 points higher at the high dose, but their GSIS will just increase proportionally to handle the load to avoid runaway glucose levels.
This is why Wheat Belly comes across (well one of the reasons anyway) so disingenuously to me. It is not readily apparent to a casual reader that he, himself, is a diabetic. Sometimes he mentions it, sometimes not. He'll make statements such as a typical glucose response to a bowl of oatmeal is in the 170's, but he doesn't always clarify, and is often less specific than the example I'm about to give. This post is typical of Davis' glucophobic hyperbole: Oatmeal: Good or bad?
If you are not diabetic and have a fasting blood sugar in the “normal” range (< 100 mg/dl) , you will typically have a 1-hour blood glucose of 150-180 mg/dl–very high. If you have mildly increased fasting blood sugars between 100 and 126 mg/dl, postprandial (after-eating) blood sugars will easily exceed 180 mg/dl. If you have diabetes, hold onto your hat because, even if you take medications, blood sugar one hour after oatmeal will usually be between 200 and 300 mg/dl.
This is because oatmeal is converted rapidly to sugar, and a lot of it. Even if you were to repeat the experiment with no dried or fresh fruit, you will still witness high blood sugars in these ranges. Do like some people and pile on the raisins, dried cranberries, or brown sugar, and you will see blood sugars go even higher.
Even if the spike is as high as he says, it won't stay up there very long in a non-diabetic, but he's likely wrong that the spike would go much higher in the non-diabetic with other stuff added, because these people will simply secrete more insulin to keep that from happening.
There is NO evidence in the scientific literature, physiology texts or any similar source that I've come across to support the exhausted pancreas theories espoused in low carb circles. It matters not how many repeat this meme, it doesn't make it so, and the onus is on those making the claims to back them up. Eating sugar or carbohydrates in general does not cause diabetes. The pancreas has more than enough insulin making capacity to last more than a lifetime. It's not like eggs in your ovaries as I've seen the analogy drawn. Yes, with aging comes some declining function, just as sarcopenia can become an issue, but that decline is not due to having used up some insulin reservoir. Eating a low carb diet to avoid getting diabetes on this basis is, frankly, downright foolish. Equally foolish, IMO, is looking at thresholds and studies in diabetics and applying those same measures to the non-diabetic. A non-diabetic will simply rarely if ever exceed around 180 mg/dL no matter what, and this includes "compensators" -- those with IR for whom an exaggerated GSIS compensates for impaired transport to achieve normoglycemia. So long as one is not continually adding to whatever has caused the IR, there's little indication the pancreas can't keep on keeping on. Remember, the LIRKO mouse is hyperglycemic throughout most of its shortened life, but hyperinsulinemic to the bitter end. We can argue over the glucose and/or insulin being toxic in this mouse, but it's pretty clear that at least in the mouse, raging chronic hyperglycemia didn't kill off its beta cells.
In summary, then, application of thresholds and targets aimed at diabetics to non-diabetics should be qualified and are often so out of context as to be irrelevant. I would agree that maintaining more truly normal glycemic control in the diabetic -- keeping glucose spikes under 200 and 2 hr readings below 140 -- may well be a more effective means to prevent diabetic complications. I'd sure as heck aim for that myself were I diabetic. But I don't see any reason for a non-diabetic to worry or obsess over postprandial spikes exceeding that magic 140 mg/dL number. If your low carb diet has rendered your formerly non-diabetic metabolism into a functionally diabetic one, it may be time to rethink things a bit. Insulin does more than stimulate glucose transport into your cells.
Next: Blood Sugar 140: Context is Everything II: The OGTT
Next: Blood Sugar 140: Context is Everything II: The OGTT
Comments
The title is:
ß-Cell dysfunction vs insulin resistance in type 2 diabetes: the eternal “chicken and egg” question, E. Cerasi, Israel
It can be found here in this compendium of papers:
http://www.medicographia.com/wp-content/pdf/Medicographia106.pdf
Here is the summary:
The idea that type 2 diabetes (T2DM) is mainly due to insulin resistance stems from the 1930s, but became dominating from the 1980s. However, evidence since the 1960s indicates that insulin response to glucose is markedly diminished from the earliest signs of glucose intolerance. Insulin pump treatment induces near-normoglycemia in T2DM with doses similar to type 1 diabetes, indicating that hyperglycemia is caused by lack of insulin, insulin resistance acting as an amplifier. Insulin secretion is genetically controlled. T2DM risk gene polymorphisms hint toward mechanisms of reduced insulin secretion in diabetes-prone subjects, in whom insulin response decreases as the number of diabetic alleles increases. I hypothesize that the genetic background of the Beta cell determines its adaptation capacity to increased insulin demand imposed by augmented caloric intake and insulin resistance; failure to adapt eventually leads to T2DM. Therefore, I regard the “prediabetic” Beta cell as a normal cell with limited adaptability, diabetes risk being entirely context-dependent (nutritional load and insulin sensitivity). Once hyperglycemia is established, Beta cells are exposed to continuous nutrient stimulation, with consequent oxidative and endoplasmic reticulum (ER) stresses. The result is increasing functional deficiencies and Beta cell apoptosis, hence reduced Beta cellmass. Some of its mechanisms are discussed. An intriguing as yet unanswered question is whether the mechanisms of Beta cell deficit in the diabetic environment operate before hyperglycemia in overfed, insulin-resistant subjects. Therapeutic agents preventing Beta cell oxidative and ER stress could stop the progression and perhaps initiation of T2DM.
Insulin pump treatment induces near-normoglycemia in T2DM with doses similar to type 1 diabetes, indicating that hyperglycemia is caused by lack of insulin, insulin resistance acting as an amplifier.
That's a WOW. Why are not insulin levels always measured along with an OGTT for diabetes diagnosis?? Blows my mind.
Which reminds me, I've got a mitochondria paper here that needs addressing.
http://www.nytimes.com/2012/10/02/health/under-stress-insulin-making-cells-revert-to-nascent-state.html?ref=research&_r=0
"But the body can become resistant to insulin, and the beta cells of the pancreas, which produce the hormone, must work harder to compensate. Eventually, the thinking goes, they lose the ability to keep up. “We used to say that the beta cells poop out,” said Alan Saltiel, director of the Life Sciences Institute at the University of Michigan. In reality, he added, this shorthand meant “we have no idea what’s going on.” "
"In mice with Type 2 diabetes, the researchers showed that beta cells that had lost function were not dead at all. Most remained alive, but in a changed form. They reverted to an earlier developmental, “progenitor,” state. "
what is the criteria for being a diabetic? if you are IGT, you may be on the way to diabetes, although not fully diabetic. in that case you should go low carb enough that you are under 140 at 2 hours and under 120 at one hour. i am IGT and both my parents are diabetic. i am not waiting to be diagnosed diabetic to keep my blood sugar within these parameters. there have been studies pointing to those who go on to develop full-blown diabetes. if you fit the criteria, you better eat low carb.
One is something I read only once (and can't remember where), where some researchers/scientists/whatever suggested that the reason why wine and alcohol in moderation was "healthy" was that when you drink alcohol with your (possibly over-carbed) meal, the alcohol will prevent your liver from dumping the glucose out, so it prevents post-meal spikes. I'm not saying I agree, but it's definitely interesting.
The other thing is just something I've wondered about re diabetics and their problems. My mother is diabetic and has become basically blind over the years. However, there is nothing wrong with her legs, and even if her heart isn't that great, she is 94 years old. In contrast, I have a good friend who is diabetic and has neuropathy in his feet and may come to a point where he loses one of his feet. However, there is nothing wrong with his eyes. I'm intrigued why the diabetic complications are so different.
If you're IGT, what are you doing to improve your insulin sensitivity? LC in maintenance does not improve insulin sensitivity, it tends to deteriorate it over time.
Re neuropathy and other complications, those are the 64K questions, eh? I hadn't intended to look into neuropathy per se, but with this glucose issue, I was wondering if it was a direct effect of hyperglycemia.
http://www.ncbi.nlm.nih.gov/pubmed/17151305
This one compared T1 & T2. Different neuropathies for different insulin dispositions.
http://care.diabetesjournals.org/content/33/3/557.full.pdf
Here are some more studies referenced in that study;
http://www.ncbi.nlm.nih.gov/pubmed/18487478
http://www.ncbi.nlm.nih.gov/pubmed/19017778
http://www.ncbi.nlm.nih.gov/pubmed/17384342
Also, phlaunt reckons goign over 140 is a risk for heart attack. Here is the link - http://www.phlaunt.com/diabetes/14045621.php
This is a qoute from that link - "Not so surprisingly, it is when you are spending several hours a day over 140 mg/dl (7.7 mmol/L) and seeing blood sugars spiking into the truly dangerous 200 mg/dl range (11 mmol/L) that your A1c will rise into the middle 6% range and your heart attack risk and risk of other complications will start to become significant."
The following study suggests that 1hr levels in normal subjects inreases cardiovascular disease risk. :
http://care.diabetesjournals.org/content/early/2009/11/12/dc09-1342.abstract
http://care.diabetesjournals.org/content/33/3/557.full.pdf
Here are some more studies referenced in that study;
http://www.ncbi.nlm.nih.gov/pubmed/18487478
http://www.ncbi.nlm.nih.gov/pubmed/19017778
http://www.ncbi.nlm.nih.gov/pubmed/17384342
Also, phlaunt reckons goign over 140 is a risk for heart attack. Here is the link - http://www.phlaunt.com/diabetes/14045621.php
This is a qoute from that link - "Not so surprisingly, it is when you are spending several hours a day over 140 mg/dl (7.7 mmol/L) and seeing blood sugars spiking into the truly dangerous 200 mg/dl range (11 mmol/L) that your A1c will rise into the middle 6% range and your heart attack risk and risk of other complications will start to become significant."
The following study suggests that 1hr levels in normal subjects inreases cardiovascular disease risk. :
http://care.diabetesjournals.org/content/early/2009/11/12/dc09-1342.abstract
Secondly, to the point of this post series, that 140 is a biomarker -- a standardized level if you will in response to a specific dose that is probably a good indicator of acute insulin secretion/beta cell function. See figure below from Insulin/Proinsulin/etc. in Normal, IGT and T2 Diabetics.
This is not the same as saying that any postprandial glucose excursion over 140 is evidence of IGT or predictive of diabetes, etc. , and it certainly offers no evidence that the glucose level itself does anything.
However, thank you for posting this study as I think it may be helpful for folks to get a handle on their own glucose handling and at least have a guess at their insulin secretion/beta cell function. Glucose and insulin are supposed to peak at around 30 min and be on the way down by the 1 hour mark. In the IGT, the 30 min insulin is not sufficient so glucose levels continue to rise and it's not until the delayed insulin response kicks in that glucose levels start to come down. It would be interesting to see profiles for normal and IGT stratified beyond the 140 2 hr cut-off. My guess is that we would see a rightward shift (delay) in maximum pp glucose levels correlating with a shift in insulin response. This information is useful to people on an individual level.
Thinking out loud here: OGTT is a measure of pancreatic beta cell function while FBG is a measure of liver insulin-signaling function. Jenny is a MODY who if I recall correctly didn't have a FBG or HbA1c in diabetic range. Her diabetes is not diet related, she has an inherent beta-cell defect. She uses insulin and Prandin (which leads me to speculate that she's a MODY-2 : " Repaglinide (Prandin) can help the body regulate the amount of glucose in the blood by stimulating the pancreas to release insulin prior to meals. In some cases, the base line glucose levels are too high as well and insulin is required." )
Anyone at risk for T2 would probably do well to keep an eye on 1 hr and 2 hr pp glucose levels and if they see evidence for beta cell "slacking" can try things like the crash diet, a short term PSMF, etc.
Are the follwing three studies all observational as well: - http://www.ncbi.nlm.nih.gov/pubmed/18487478
http://www.ncbi.nlm.nih.gov/pubmed/19017778
http://www.ncbi.nlm.nih.gov/pubmed/17384342
I wouldn't want to bother my doctor about HbA1c, when all of my blood glucose results have been healthy, with the odd result in the mid 1hr after eating junk food. I've only been checking my blood sugar as I keep getting random spells of blurry vision, and my blood pressure is fine.
Finally, you didn't give your opinion on this study, which concerned me.
Thanks
"The insulin secretion/insulin resistance index is useful as a predictor of future development of type 2 diabetes."
I think I'll do a quick blog post on this paper in the next day or so. If insulin is a better predictor it *may* mean that it is the primary factor in the etiology. This is what I believe based on my reading of the literature (especially recently) demonstrating that postprandial insulin production is impaired early on in the progression of the disease.
All of the observational studies simply collect baseline data and look for incidence of the outcome of interest (in this case developing T2). These can only identify associations, just like all the various cholesterol tests, inflammation markers, etc. The associations can be used to generate predictive risk factors, but they can never demonstrate causation. Causation can be established (or at least to some degree) only with experiments whereby something is manipulated (preferably compared to a control group that gets subjected to the same protocol minus the treatment -- e.g. a placebo pill). However observational studies can be useful in identifying a lack of causation. For example if nephropathy is caused by hyperglycemia per se, then we should see similar patterns regardless of the cause of the hyperglycemia (poorly controlled T1 vs. T2 diabetics) but this is not the case, T1s are susceptible to nephropathy and more severe cases which would indicate that insulin deficiency may be more causative than the hyperglycemia. Hope that makes sense. Be aware that I don't think we know this to certainty.
BTW, you can order an HbA1c by mail for like $10 from WalMart. With the blurry vision episodes I'd work with your doctor to find the cause ... it seems highly unlikely your blood sugar is the issue.
Lastly on that final study, it is again an observational study. The interrelationships between hormones and inflammation, etc. are very complicated, but yeah ... taken together that 1 hour pp glucose level may be the simplest indicator (as proxy for insulin secretion) of things going wrong early.
Post a Comment
Comment Moderation is ON ... I will NOT be routinely reviewing or publishing comments at this time..