Biomarkers: Context and Are They Causative Agents?
I received a comment recently on the Blood Sugar 140 series that prompted this post. Actually, it prompted a post on the best predictor for T2 which will be forthcoming, but in fleshing out some background for that, I realized it was worth a post on its own. Below are links to previous post series I'm referring to:
- Blood Sugar 140: Where did the 140 mg/dL threshold come from?
- Blood Sugar 140: Context is Everything I - Diabetic vs. Non
- Blood Sugar 140: Context is Everything II: The OGTT
- Blood Sugar 140: Diabetic Neuropathy, Is it All About Hyperglycemia?
"Cliff Notes" Blood Sugar 140: There is a commonly repeated "fact" out there that blood glucose levels over 140 mg/dL lead to nerve damage (and organ damage) generally attributed to the process of glycation. Also implied in this is that such damage is cumulative such that any excursion over 140 is inflicting a little damage along the way. This traces back to the following page on Jenny Ruhl's website: Research Connecting Organ Damage with Blood Sugar Level:
The studies you will read below, some of which are not cited in the AACE guidelines, make a cogent case that post-meal blood sugars of 140 mg/dl (7.8 mmol/L) and higher and fasting blood sugars over 100 mg/dl (5.6 mmol/L) cause permanent organ damage and cause diabetes to progress. {emphasis mine}
One of those studies is this one: Increased Prevalence of Impaired Glucose Tolerance in Patients With Painful Sensory Neuropathy. I discussed the issues with the interpretations of this study in the first installment above and won't rehash them all here. But it is a classic case of misinterpretations at several turns. The study started with a group of older people with "idiopathic neuropathy" (no known cause) and discovered that it turned out that 18% were actually diabetic and didn't know it, and half had impaired glucose tolerance, IGT. Note that this would leave roughly one-third of patients with neuropathy who had normal glucose tolerance.
Now IGT is diagnosed with a standard oral glucose tolerance test, OGTT, and the 140 mg/dL was the cut-off for the diagnosis at the 2-hour post ingestion mark. There was no control looking at the prevalence of diabetes and IGT in a similarly aged group of non-neuropathic people. Further, which is a point I cannot drive home frequently enough,
The 2 hour glucose level after ingestion of a standard dose of glucose is a biomarker that is essentially meaningless taken as an instantaneous/isolated data point.
I hope by drawing parallels to another metabolic bogeyman of low carb advocates, triglycerides, to demonstrate the folly of taking such biomarkers out of context and drawing conclusions that are inappropriate in addition to being of highly speculative and/or scare-mongering nature.
According to the American Heart Association, normal fasting triglycerides are under 150 mg/dL. Out of thin air it seems that low carb advocates have decided that under 100 mg/dL is optimal, so you can use that value if you like. Those wary of the linkage of LDL levels to CVD are quick to point out that triglycerides are a better biomarker for risk. They generally are, but LDL-P and apoB give that biomarker a run for the money. Back to the trigs ....
It doesn't get talked about much, but postprandial lipid handling may be as, if not more important than fasted lipid profiles in terms of characterizing one's metabolic health. The following study offers some insight: Relation of Triglyceride Metabolism and Coronary Artery Disease. Studies in the Postprandial State. This study is similar to the neuropathy study in a way in that they started with subjects manifesting an outcome (in this case CAD) and looked at metabolic function. Only here they looked at lipid handling instead of glucose handling. Subjects were administered a "fat load" (...whose ingredients have been described contained 729 kcal per square meter of body surface and consisted of 5.3 g protein, 24.75 g carbohydrate, 240 mg cholesterol, and 65.2 g fat (from heavy whipping cream) with a polyunsaturated to saturated fat ratio of 0.06. This test meal was employed because in previous studies, it gave rise to a postprandial lipemia whose magnitude varied greatly among individuals but was very constant within a given subject. ... Using values from here, if the average body surface area is 1.7 sq.m. the fat load administered was ~110 grams. )
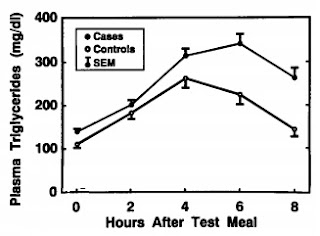 At right is the 8 hour time course of postprandial triglyceride levels. In the controls, triglycerides peak around 4 hours and begin to drop, while in the CAD group, triglycerides continued to rise through 6 hours before falling, and not returning to anywhere near baseline when control levels roughly do.
At right is the 8 hour time course of postprandial triglyceride levels. In the controls, triglycerides peak around 4 hours and begin to drop, while in the CAD group, triglycerides continued to rise through 6 hours before falling, and not returning to anywhere near baseline when control levels roughly do.
I would note that the normal peak is around 250 mg/dL while the CAD group exceeds 300 mg/dL at this time point and reaches about 350 mg/dL. I would also note that even in the controls, triglycerides had not returned to baseline after 8 hours and in those with CAD? Their postprandial triglycerides remained higher than the controls' peak at the 8 hour level.
If triglycerides = bad, then this is sobering news indeed. Drawing parallels to the OGTT, if this were a standardized fat tolerance test, I'll call it an OFTT, one could envision that diagnostic cut-off criteria could be established at 4, 6 and 8 hours post-ingestion. A reasonable criteria for IFT (impaired fat tolerance) might be a 6 hr trig level off over 300 mg/dL and an 8 hr trig level over 200 mg/dL. Now let's suppose that based on these results and a few others I were to write the following:
The Peril of Triglyceridic Excursions
Another factor affecting the healthfulness of fat consumption is the degree to which blood triglyceride levels fluctuate. Blood triglyceride levels should remain somewhat stable at under 150 milligrams per deciliter. After eating fat, the blood triglyceride level should rise no higher than about 200 milligrams per deciliter and should return to normal levels within eight hours.
When blood triglyceride levels move outside the healthy range, significant health problems can follow. Indeed, mortality rates are lowest when both fasting triglyceride and two-hour postmeal blood triglyceride levels are between 101 and 153 milligrams per deciliter; higher blood triglyceride levels are associated with an increased risk of death.
Hypertriglyceridemia— blood triglyceride levels that are too high— is common in people with coronary artery disease and leads to cardiac damage and heightened mortality rates. Even in those who don't yet manifest signs of coronary artery disease, postprandial (after-meal) surges in blood triglycerides cause atherosclerosis and greatly increase the risk of coronary artery disease and myocardial infarction. To avoid these risks, it’s important to keep postprandial (postmeal) blood triglyceride levels below 200 milligrams per deciliter. Failing to do so may damage your arteries, little by little, every day.I would be (rightly) trounced for engaging in hyperbole and misinterpreting scientific research. Such justifiable criticisms would no doubt be accompanied by accusations of having a fat phobic agenda clouding my cognitive processes ... more likely less kind words would be used and I'd be called a stupid idiot who can't understand what I'm reading on PubMed. I'm just trying to scare people away from eating fat, and I want them to be fat and diabetic and sick so I can sell them pharmaceutical drugs that I probably own a ton of stock in ... oh ... and selling books by trying to scare the bejeebers out of people.
Come on ... you know that is true.
So I'm sure reading through that many began thinking of what was wrong with what I wrote. I'll suggest a few:
- Postprandial and fasting levels are not the same thing so fasting triglyceride levels are irrelevant to postprandial levels.
- Nobody eats 100g of fat in one sitting so this test is irrelevant.
- The normal controls had triglyceride levels of 250 mg/dL at the 4 hour mark so the 8 hour OFTT of 200 mg/dL doesn't mean that triglycerides should never go above 200 mg/dL.
I'd also point out a couple more
- Look at that! If you eat fat all day, your triglycerides are never going to come back down above dangerous levels ... oh wait ... that would apply to glucose levels and fasting glucose and insulin and ... nevermind ... move on please ....
- The CAD group had normal to borderline high fasting triglycerides according to AHA guidelines, so the fasting triglycerides are a poor indicator of CAD risk after all and as utterly useless as LDL. My triglycerides are low on my LCHF diet so I'm protected frrr ... oh wait ... nevermind ... this one doesn't fit my biases ... move on ...
- Some carbohydrate was included in the OFTT and we know insulin traps fat in the fat cells so this irrelevant to my low carb high fat diet as the triglycerides wouldn't be trr... oh wait ... nevermind ... this one might not work out in my favor ... move on ...
So ....
One of the themes that is emerging with the diabetes reviews I've been going through lately is that postprandial diagnostics seem to be far better for identifying the early stages in the etiology of diabetes compared to fasting diagnostics. These continue to point to postprandial beta cell dysfunction as being the primary "defect" that initiates the cascade in deterioration of glucose (and likely lipid) regulation, and I will be discussing this moving forward here. Before summing up, I think a nice juxtaposition of what impaired glucose clearance and impaired fat clearance looks like is worth showing here:
On left we have glucose levels following an OGTT for normoglycemic individuals (bottom curve) and those with impaired glucose tolerance. At right are triglyceride levels following an OFTT in normal controls and CAD cases as shown. These populations are not equivalent, but both profiles show what impairment of postprandial nutrients looks like. The timeframes differ due to the differing digestion/absorption rates and thus appearance of glucose and lipid in circulation, but four similarities can be seen: (1) delayed maximum, (2) higher peak concentration, (3) levels remaining substantially above baseline at time points by which normal individuals achieve roughly baseline levels.
Biomarkers Context and Causation
Within my lifetime, medicine has undergone great changes. Around when I was born, a person had a heart attack and if they survived the focus was on preventing the next one. Doctors being thinking and feeling humans with loved ones just like the rest of us -- especially the surgeons who just patched up the "wounded" -- hoped to be able to improve their patients' lives by helping them never have that heart attack in the first place. Scientists began looking for factors that could be used to assess risks in the hopes that through lifestyle choices people could minimize their risks. And so it went where associations between TC and LDL and CVD were found, and all manner of factors and proteins and glucose levels etc.etc.etc. have been studied to look for correlations. The hope was that those correlations might be found such that we could measure someone's levels at age 20, assess their risk of having a heart attack at 60 and identify lifestyle interventions to minimize that risk.
Now I'm fully in agreement that the major first foray into biomarker medicine has been an unmitigated disaster. High "cholesterol" is associated (still rather closely) with atherosclerosis. This evolved into the meme that cholesterol "clogs" your arteries and, worse still, that dietary cholesterol (like that in eggs) was responsible for high levels in the blood. Then the obvious intervention was to reduce cholesterol consumption and if that failed, medications (and don't forget supplements) were developed to lower it artificially. However scientists kept toiling behind the scenes trying to elucidate the mechanisms by which "cholesterol" might be causing atherosclerosis, ever mindful that not everyone with high cholesterol died of a heart attack and not everyone who died of a heart attack had high cholesterol. They went looking for better biomarkers -- and so now we have TC, LDL, HDL, VLDL and further subfractions of all the L's by particle size and number and we have proteins like apoB associated with the L's or not ... and on and on ... and great strides have been made in identifying more robust predictors. We're still floundering as to what to do with those, and sorry butter drinkers, but you are no more assured of being right in your chosen solutions.
There's no evidence that avoiding eggs at 30 staved off heart attacks by 60. So too, there is no evidence that avoiding carbs at 30 will have any impact on whether or not you develop diabetes by 60. Blood cholesterol levels and blood glucose levels are biomarkers. To be taken in context. And they are largely governed by the state of one's metabolic house independent of diet. Where they have been shown predictive of the future, it is in the degree to which they shine a light on the underlying metabolic health (e.g. pancreatic function) ... yet all of these have their limits.
An isolated blood glucose level of 150 mg/dL, even several times per day, can no more be implicated in causing neuropathy than an isolated triglyceride level of 300 mg/dL, even several times per day can be implicated in atherosclerosis.
So, by drawing the parallels that I did in this post, I hope to encourage critical thinking and bring a degree of internal skepticism to this community. Too often, utilizing far greater levels of hyperbole, statements such as my hypothetical above are made on blogs and in the books of "experts" and "gurus" in this community. Sadly, all too often, such statements are accompanied by a litany of peer review literature citations and presented as settled science. I can understand economies of words in blog posts and such, and even in more formal works like books in order to make the information more accessible. It is when doing so alters the validity of the statements such that it misrepresents the scientific substantiation for them that there is a problem. Especially when such information is presented as the "correct" settled science and presented in such a manner as to be better than that inferior knowledge and understanding of the science that your doctor or the mainstream establishment, or, even the (corruption implied) scientists themselves possess.
There is much merit to many of the ideas circulating in this community. Only in marrying those ideas with what the science taken as a whole shows us, and in working with current establishments to effect change can true change to the benefit of all be achieved. That sounds all kumbaya, but the current approach of demonizing doctors and scientists as unfeeling drone agents of The Man who want you to be sick and diabetic for their fun and profit is not the way to go. At the end of the day, the demonizers turn out to be largely interested (some more overtly than others) in notoriety, book sales, subscription fees, and seminar admissions ... and the cashiest cow of them all: supplements. Supplements for when that diet you were told is the most optimum of all diets falls short of expectations or even makes matters worse.
I suspect one reader of this blog recognized my hypothetical writings, because reworking that part of Perfect Health Diet should be relatively fresh in Paul Jaminet's mind. Those statements are similar to what is written in the new 2012 edition at Kindle Edition locations 1767-1781. The wording was an improvement on the verbatim conclusions drawn by Jenny Ruhl, but still not accurate interpretations of what the supporting scientific literature demonstrates. The original excerpt:
The Peril of Glycemic Excursions
Another factor affecting the healthfulness of carbohydrate consumption is the degree to which blood glucose levels fluctuate. Blood glucose levels should remain in a stable range,
between about 85 to 105 milligrams per deciliter. After eating carbohydrates, the blood glucose level should rise no higher than about 140 milligrams per deciliter and should return to the normal range within a few hours.
When blood glucose levels move outside the healthy range, significant health problems can follow. Indeed, mortality rates are lowest when both fasting blood glucose and two-hour postmeal blood glucose levels are between 81 and 108 milligrams per deciliter; both lower and higher blood glucose levels are associated with an increased risk of death. 18
Hyperglycemia— blood glucose levels that are too high— is common in diabetics and leads to organ damage19 and heightened mortality rates. 20 Even in nondiabetics, postprandial (after-meal) surges in blood glucose cause nerve damage21 and greatly increase the risk of stroke22 and cancer. 23 To avoid these risks, it’s important to keep postprandial (postmeal) blood glucose levels below 140 milligrams per deciliter. 24 Failing to do so may poison the nerves, little by little, every day.
I would point out that the book goes on to state that VLC is not the solution, but despite its more moderate stance on dietary carbohydrates, the basic premise of PHD is that there is a "sweet spot" of carbohydrate ingestion where too little and too much both lead to adverse effects. I disagree, and ironically much of the science put forth in PHD does as well.

Comments
I believe there is a downside
Look into my homepage ... having trouble getting pregnant with second baby
2. Glycation gets out of control with chronically elevated glucose levels. I've not seen any level cited in the peer review as a threshold. It seems a plausible mechanism for some things but again, there's little if anything in the literature elucidating said mechanism.
Thanks
I had an eye test but only came up as having problems with short distance vision. In actuality, I'm having problems with long and short vision. It is just a general blurry vision and dizziness.
You know, Jenny Ruhl is a MODY which means she has a genetic defect, and it seems that with MODY it just takes some time for the hyperglycemia to present and/or to be detected. This could be your situation as well. MODY-2 is a signalling issue, not a beta-cell capacity issue and I suspect this is Jenny's form as she has discussed taking Prandin (and how this will not work for most other forms of diabetes).
If it seems that you have the reaction to very many foods, then maybe you have leaky gut, wherein the increased intestinal permeability allows large molecules (notably proteins and peptides) to enter the bloodstream that ordinarily shouldn't.
If you search for a connection with your symptoms and food sensitivity, you'll find alternative health sites discussing blurriness and dizziness. Just because a lot of that alternative stuff is wacky doesn't mean that it's all wrong.
Regarding BG, the main question I'd pursue is whether the changes in the lens' shape caused by changes in their water content (caused in turn from excess BG) could come on so quickly and go away so quickly. A patients group could be a good place to ask, since they'd be familar with practical matters like that, though maybe not quite so versed in the science and mechanisms.
I've been looking into food allergies. It's been difficult, as I'm a big guy `and I snack a lot. I've had to separate the snacks into individual foods, to find the trigger foods.
ping cream (39.5% fat), two tablespoons of chocolate-flavored
syrup, one tablespoon of granulated sugar, and one tablespoon
of instant nonfat dry milk. Of the 1,362 calories, 2.8% were de-
rived from protein (9.5 g), 14% from carbohydrate (48 g), and
86%frorn fat(l30g). Cbolesherolcontentwas480mg, andthe
ratio of polyunsaturated/saturated fat was 0.059. Ingredients
were mixed but not blended so as to obtain a readily drinkable
liquid. The test meal was administered per 2 m’ of body surface
to adjust adequately for major variations in blood volume (Ill).
That's from tracing back to 1983, http://www.ncbi.nlm.nih.gov/pmc/articles/PMC393615/?page=2
The same Herr Patsch as the author.
The high after-meal levels of fat correlate with heart disease. Note that the study is from around 1990.
Congratulations on turning yourself around. Did you use any particular diet?
In any case, I put a bunch of links in one post in the library and there's one with best predictor in the title that I plan to blog on -- at least briefly. In that study, insulin secretion index was the best predictor for developing T2 vs. baseline and 1 hr glucose (though not tabulated) was somewhat dubbed a runner up. I think any single level of a biomarker is not all that helpful, but I can say with almost absolute certainty (based on what the science shows with nary a black swan to be seen) that the insulin secretion begins to go first. The 1 hr level would be related to the insulin secretion far more than the 2 hr level which may be complicated by endogenous glucose production so this all seems to be pointing in that same direction.
If I were at risk, as I know you have mentioned, I might do 1 hour glucose tests with some fixed amount of the same carb from time to time. If the level increases at the 1 hour mark with time, this would be evidence that insulin secretion is likely impaired somewhat. This seems to happen to just about everyone as we age anyway, so I wouldn't panic, but if it seemed to be accelerating I'd look for reasons why, and/or get the insulin secretion measured directly (and proinsulin if I could get it).
One final thing I'm not sure on is, in some post-prandial readings, I have gone from quite high (7.5-9.5) to low (3.9-4.3) within 30-60 mins. Could I have gone through a reactive hypoglycemic dip in that 30-60 min period and rose back up again?
Post-Prandial Hyperglycemia or Hypoglycemia were the two things I set out to investigate when I bought a BG monitor. I passed my personal OGTT test and have passed all food tests. I've been checking Blood Pressure as well. Basically, I've been trying to rule out all options before asking about an allergy, as allergies are quite rare. Plus, last time I asked about an allergy my doctor dismissed me , suggesting I am too old to develop an allergy.
Your food testing would now center on the glycemic effects of the foods, and also on the insulin index:
http://www.ajcn.org/cgi/reprint/66/5/1264.pdf
(Btw, allergies can develop at any age, though that's not common.)
Also, be vary wary of blacking out and cracking your head from falling. If you feel faint. drop your center of gravity and hold into something.
I thought of ditching the widget entirely as post title and name is pretty lame, but at least it alerts those interested to comments on older posts.
Are you getting the same readings 3-4 hours after eating 130g of oats? If so, you have IGT. I got very similar readings during a 5 hour OGTT when I had IGT.
It's got nothing to do with phytic acid, which impairs protein digestion & mineral absorption.
3.9-4.3mmol/L isn't hypoglycaemia.
The BG swing, Michael, is unlikely to be caused by a food allergy though. Anything is possible, but I'd test some different carbs and see if the effect is the same.
Thanks
On a related note, I just remembered there was a Reactive Hypo on Jimmy's forum who commented here a few times too. He reported that honey and fruit were better for his blood sugar than starch. Maybe worth investigating.
Post a Comment
Comment Moderation is ON ... I will NOT be routinely reviewing or publishing comments at this time..